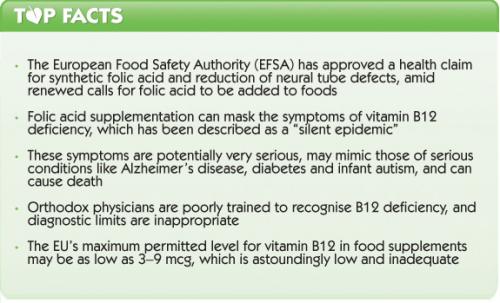
As the European Food Safety Authority (EFSA) finally approves a health claim for folate supplementation, amid new calls for folate fortification in Europe and beyond, the widespread and associated problem of vitamin B12 deficiency is being overlooked.
Folic acid supplementation can mask vitamin B12 deficiency
EFSA’s approved health claim for folate – in reality, synthetic folic acid, a very different beast indeed – belatedly recognises the nutrient’s key role in preventing neural tube defects (NTDs) in developing foetuses. Positive as this development may be, however, renewed calls for folic acid to be added to foods are somewhat simplistic.
Considering folic acid in isolation is a limited approach that fails to take into account its combined and synergistic action with other nutrients and cofactors, including other B vitamins. Vitamins B6, B12 and folate, otherwise known as B9, all work together and supplementation of any one of them may lead to a serious imbalance. Deficiency of serum B12 or folate can cause red blood cells to enlarge, a condition known as megaloblastic anaemia. Taking synthetic folic acid alone can mask symptoms of B12 deficiency, as folic acid can cause the blood cells affected by B12 deficiency to return to normal. The presence of enlarged blood cells is used to determine vitamin B12 status, despite the fact that deficiency and associated symptoms can occur below the level at which blood cells are affected. The result, regardless of the presence of enlarged blood cells, is that a potentially serious B12 deficiency may remain undiagnosed.
Vitamin B12 deficiency: the hidden epidemic
A further serious concern is that patients with vitamin B12 deficiency are frequently misdiagnosed, because the condition mimics many other conditions such as depression, psychosis, multiple sclerosis, chronic fatigue syndrome, early Parkinson’s disease, diabetic neuropathy and Alzheimer’s disease. In babies, B12 deficiency symptoms can mimic those of autism.
The serious problems caused by undiagnosed and misdiagnosed B12 deficiency, compounded by healthcare strategies that exacerbate the problem, reveal that Western healthcare systems are seriously failing patients. Orthodox physicians are inadequately trained to consider or recognise nutritional deficiencies, even in those who are most at risk. Diagnostic testing for B12 deficiency is inadequate and inappropriate, with many doctors failing to match blood results with the patient’s clinical picture. The lower limit of normal for serum vitamin B12 is much too low (see Call to Action, below), and clinical guidelines and protocols are failing to address the problem.
B12 deficiency is emerging as a serious, hidden epidemic among all ages, yet it is an easily preventable nutritional problem — solved simply by ensuring that the patient receives adequate vitamin B12, often given as regular injections, at little cost!
Who is at risk of B12 deficiency?
The most frequent cause of B12 deficiency is malabsorption, which may be caused by low stomach acid, a lack of intrinsic factor and/or suboptimal pancreatic, small intestinal or liver function. Those most at risk include:
- Those who have adopted a vegetarian, vegan or macrobiotic lifestyle
- The elderly and people with eating disorders, such as anorexia nervosa or bulimia
- Those taking certain medications, including laxatives, antacids and metformin, or those who have been exposed to nitrous oxide
- Pregnant and nursing mothers
- The offspring of those already deficient
- Heavy drinkers and smokers
- Those with high homocysteine
- Those with gastrotintestinal disorders, including autism, or those who have had gastric surgery
- Those taking high doses of folic acid
- Those with autoimmune disorders
Passionate campaigners
As one might expect, there are dedicated people out there who are trying hard to change this sorry situation. Sally Pacholok, a trained emergency nurse from the US, is among the pioneers in the field. Along with her co-author, osteopath and emergency physician Jeffrey Stuart, her book Could It Be B12? An Epidemic Of Misdiagnoses broke new ground when first published in 2005. Pacholok became passionate about the issue of B12 deficiency because, “In 1985, [she] diagnosed herself with vitamin B12 deficiency, after her doctors had failed to identify her condition. As a result, she is passionate about the need to educate the public about the dangerous consequences of this hidden and all-too-common disease.” Today, Pacholok and Stuart run the B12 Awareness campaign, whose mission statement is simple: “Unmasking the epidemic of undiagnosed vitamin B12 deficiency through education and advocacy”.
Sally has taken her cause across the Atlantic. In 2009, she and Stuart organised ‘B12 Awareness Week’ in both the US and the UK, the latter in collaboration with Martyn Hooper, Executive Chairman of the UK’s Pernicious Anaemia Society (PAS). The B12 Awareness Campaign’s strategy, according to Pacholok, is to use the legislative process to make a ‘B12 Awareness Week’ – or even Month – a yearly event in the US.
A worldwide campaign
In the UK, at least, Pacholok isn’t alone. The B12 deficiency Support Group (B12d), now a charity, was set up in 2006 by UK general practitioner (GP), Dr Joseph Kayalackakom – Dr Chandy to his friends – and his assistant, Mugo Minney PhD, with broadly similar aims to Pacholok and Stuart’s B12 Awareness campaign. Despite some success, it’s clear that there’s still some way to go before B12d realises its aim of wider recognition and treatment of vitamin B12 deficiency on the UK National Health Service (NHS). A recent review of the ‘clinical knowledge summary’ – basically the evidence base – for B12 deficiency concluded there was no need for major revision, despite the present clinical recommendations dating back to 2007–8. But with Dr Chandy enjoying a higher profile both in the UK and his native India, including a meeting with UK Prime Minister David Cameron, things may be looking up.
EU vitamin harmonisation
A number of European Union (EU) Member States, in particular Germany, Denmark and France, have long pushed to ensure an extraordinarily low maximum dosage for vitamin and mineral food supplements. Germany has, for example, been successfully challenged in the European Court of Justice (ECJ), by none other than the EU Commission. In 2005, the German Federal Institute for Risk Assessment (BfR) published a 222-page document justifying what it considered as maximum levels for vitamins in foods. Astoundingly, it proposed a maximum level of 3–9 micrograms (mcg) of vitamin B12, despite copious evidence that dosages well over 1000 times greater than this have never been shown to have adverse effects.
Following a case brought to the ECJ against the French Government by Solgar France and other food supplement interests, the European Commission is legally bound to introduce EU-wide harmonised legislation setting both maximum and minimum amounts for vitamins and minerals in food supplements. As exposed in two peer-reviewed scientific papers authored by ANH-Intl executive & scientific director, Robert Verkerk PhD, the methods being considered by the Commission for establishing maximum permitted levels (MPLs) are flawed. ANH-Intl is now imminently poised to commission an independent research institute to help develop a novel, science-based approach to both risk and benefit assessment that could form the basis for harmonisation. We’ll report on this in due course.
However, one thing of which we can be fairly sure is that such a new approach will not limit vitamin levels unnecessarily or irrationally. It becomes increasingly clear that Germany and other governments that have limited vitamin B12 in food supplements have done so to protect vested or pharmaceutical interests, rather than for reasons of public safety.
Call to action
- If you or anyone you know has a constellation of symptoms similar to this, consider B12 deficiency as a priority!
- Remember that animal products are the best sources of vitamin B12, especially organ meats, beef, chicken, fish, shellfish, pork, dairy and eggs
- Orthodox medical diagnosis of B12 deficiency is via a blood test, and Sally Pacholok warns that the reference ranges used are too low. She recommends treating for B12 deficiency below a level of 450 nanograms/L (ng/L); the US lower limit is 200 ng/L (expressed as 200 picograms/mL [pg/mL]) and the UK’s is 150 picomol/L (equivalent to 200 ng/L). If your tests show a level below 450 ng/L, which is approximately equivalent to 340 picomol/L, Pacholok suggests that you consider B12 supplementation after visiting a suitably qualified healthcare practitioner.








Comments
your voice counts
09 September 2013 at 5:00 pm
Most B12 deficiency is caused by MTHFR mutation. Sooo glad I now know what has been wrong with me. It doesn't matter how much B12 I take in, I cannot metabolise it unless it is methyl. Folic acid is not natural and poisons those with MTHFR mutations. 90% of the folic acid just stays in our bodies poisoning us.Folate is what out bodies need never folic acid.
B12 as methylcobalamin and folate as 5 methylfolate
NEVER take cynocobalamin
09 September 2013 at 5:41 pm
This problem is often caused by genetic mutations that affect the methylation process. Isn't it about time they started testing for these and treating individuals appropriately? Folic acid fortified foods and supplements can make the problem worse. These individuals need to be treated with folate and methylcobalamine and possibly starting with small doses, as the conversion pathways may be blocked.
09 March 2014 at 10:34 pm
Re video on Vit B 12 deficiency.
I cannot view it because when you press play it comes up with the words 'This video is private'.
I have seen it before and wanted to see it again and pass it on.
Do you know why it is now unavailable?
12 March 2014 at 12:11 pm
Hi Helen, I'm not sure what they were doing but its back up now and available to view!
02 November 2014 at 2:51 pm
Hi,
My B12 level is arround 280. Earlier it was 190. Since than I have been taking B12 injections and i am happy that the B12 level has risen to 280. But I still feel very lethargic and doesn't feel like doing anything because of low energy. What should I do?
I still get cramps in my legs for minute physical activity like sitting and when i lift my leg up while doing yoga. Basically which ever activity flexes my leg muscles i get cramps and at times in my lower back and facial muscles too. Is there any way by which i can reverse these effects or can become fit enough to at least do normal yoga.
I can't believe that i got B12 deficiency as i am an avid food lover and mainly prefer eating Non-veg and that is why my doctor initially suggested uric acid test for joint pain.
Plz guide me how to reverse the damages that i got due to B12 deficiency.
Regards,
Raj Rai
03 November 2014 at 11:36 am
Hi Raj
Thank you for your comment. We're sorry to hear about your troubles but unfortunately, as a campaign organisation, we're unable to give medical or health advice. We'd suggest you try and see a doctor who could advise you appropriately. Depending what country you are in, here are some links to institutes/societies with lists of doctors that could help you:
UK - British Society for Ecological Medicine (http://www.bsem.org.uk/resources/find-a-practitioner/)
US - the Institute for Functional Medicine (https://www.functionalmedicine.org/practitioner_search.aspx?id=117)
Australia - Australasian Integrative Medicine Association (https://www.aima.net.au/profiles/search/).
Hope this helps!
18 May 2015 at 3:59 pm
Not sure if this helps or if anyone is interested but I recently heard about a new oral prescription alternative to the injections called Eligen B12. I recently read that it works even if you don't have intrinsic factor (so even if you don't have normal gut absorption). Apparently it came out a month or two ago. Has anyone heard of it or tried it??
21 May 2015 at 11:03 am
Hi,
I have a long list of diagnosed illnesses. NHS fails in every regard and there is no treatment - what they do offer is toxic. ME/cfs, fibromyalgia, hypertension, vomiting-diarrhoea-migraine effected by what I eat,carbohydrates/sugar induce these symptoms so are avoided the result is fewer ill sessions. Malnourished, malabsortption, hypertension, neuropathy in my finger tips, etc.
TWO ITEMS THAT WERE BENEFICIAL
BioCare B12liquid, taken orally which is absorbed straight into the blood system. I also rubbed some of the liquid into my finger tips and within 5 minutes the pain reduces.
Magnesium Chloride crystals in a bath soaking for 20-30 minutes this allows the body to absorb the magnesium needed and gets to the muscles and tendons quicker. The pain has reduced, the hyperactivity in my body has been reduced. I feel much calmer and am in less pain. I am beginning to feel a little bit more normal. I have been doing this for a month now, its really good and I intend to continue.
Hope this is useful to you.
Vi
23 September 2015 at 4:38 am
Not sure where the idea came from that supplementing with folic acid is bad. Several studies have shown that even at high doses of folic acid over 99.9% is converted to active folate analogues. FYI whilst some food contain predominantly 5MTHF, the majority contain less than 50% of the folate as 5MTHF. You do need though to have both intracellular folate and vitamin B12, homocysteine and MMA tested to determine true deficiency. Data suggests that even at 300 pmol/L for B12 this may result in sub-clinical deficiency.
25 September 2015 at 9:38 am
The prime concern with high dose folic acid used long-term is linked to a range of issues which include masking B12 deficiency, through to cancer progression, accumulation of unmetabolized folic acid (UMFA), impacts on polymorphisms e.g. DHFR. Some of these issues are considered in: <a href="http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4287316/"; target="_blank" rel="nofollow">http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4287316/</a>;. If you search for unmetabolized folic acid in PubMed you will find other relevant papers. We agree that 5-MTHF and 5-FTHF may be lower in food folate and bioavailability of food forms is <a href="http://jn.nutrition.org/content/135/5/1139.long"; target="_blank" rel="nofollow">only about 50%</a> that of synthetic folic acid. But that is one reason UMFA from folic acid supplements and fortified foods is a problem as there is no buffer. If there is a SNP on DHFR, that <a href="http://jn.nutrition.org/content/145/3/387.full.pdf+html"; target="_blank" rel="nofollow">may make matters worse</a>. Hope this is useful.
11 December 2016 at 3:09 am
I have two MTHFR defects. Food fortification IS BAD. People like myself, can NOT use this form of folate, and it makes us very sick. It stops us using the real folate. With these genetic defects, at present I only use 30% of real folate in food, and by eating foods with folate fortification (of SYNTHETIC folate), it blocks my uptake of the folate, real folate that I can use. I am OPPOSED to any meddling of our food, in any shape or form. I have been sick for damn 20 years, I had no idea, that the nitrous oxide I had for third baby, send me nuts, had no idea that the folate supplements I used in pregnancy, contributed to two babies with heart defects. [email protected] Attempting to regain my health age 57, was bedridden, for a damn B12 deficiency, never tested for previously? Thankyou so much for your wonderful video, you have saved my life.
03 May 2016 at 6:41 pm
I have watched the video many times. Finally, it makes sense. No one in the medical field would listen. 5 doctors. My Doc's an idiot. Knew my b12 was low 6 year ago, just told me 2 weeks ago(dismissively). In Hospital 2 x in the last year, both times a week. Massive seizure, big memory gaps for years, no strength,numbness in hands and feet, cognitive deficits, neurologist put me on folic acid alone for a year, really went downhill. Now I need a walker (i'm 50 ). After taking B12 1000mg for 2 months, I can think again. But I'm stunned and angry when I look in the mirror, and my neurologist just said he thinks its all in my head. Where? Next to the lesion on my brain ? Beside my degenerating spine? Can some one out the help me? I feel like I going crazy. I'm not a stupid person, i'm pretty resilient, and I've never kicked a cat. Anyone out there?
11 December 2016 at 6:20 am
Check your MTHFR genetics. ONLY take the correct B12 supplements, I suggest injections. I had ONE injection, and was the ""light bulb moment"".......... The B12 injections are $8 for three, so cheap. No money for pharma perhaps? I now intend to have injections once a week for about three months, then perhaps switch to tablets. If you have been low for 6 years, like I have been for at least that long, takes time for the cellular repair to happen. Good luck! So sad, now to realise my mother suffered long and hard with B12 deficiencies, untreated, alzeimers..............
Your voice counts
We welcome your comments and are very interested in your point of view, but we ask that you keep them relevant to the article, that they be civil and without commercial links. All comments are moderated prior to being published. We reserve the right to edit or not publish comments that we consider abusive or offensive.
There is extra content here from a third party provider. You will be unable to see this content unless you agree to allow Content Cookies. Cookie Preferences