“The United States spends more on health care than does any other country, but its health outcomes are generally worse than those of other wealthy nations. People in the United States experience higher rates of disease and injury and die earlier than people in other high-income countries”. ‘Nuff said. But what are the reasons?
US healthcare system examines itself
The quote above comes from a JAMA article commenting on a recent US National Research Council/Institute of Medicine (NRC/IOM) report entitled Shorter Lives, Poorer Health. The report doesn’t examine the costs of the US healthcare system itself, instead focusing on what it terms the ‘health disadvantage’ suffered by north Americans.
The ‘health disadvantage’
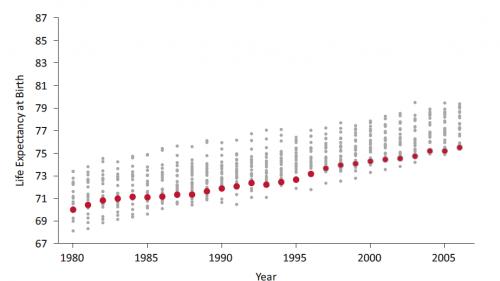
The US health disadvantage is a many-tentacled beast. Most strikingly, US citizens have shorter life expectancies than people in most of the wealthy countries selected for comparison (Figure 1; see relative positions of red dots for US, and grey dots for 21 other countries). Compared with other wealthy countries, US adolescents have higher rates of motor vehicle fatalities and homicide deaths. Infant mortality is higher in the US than in any other high-income country. US rates of diabetes and obesity are the worst among the comparison group, while the US fares below average in terms of chronic lung disease, heart disease and disability rates.
The report even notes that, “The nation’s large population of recent immigrants is generally in better health than native-born Americans” – a fact pointed out by our colleagues at ANH-USA already. And unfortunately, President Obama’s recent healthcare reforms are likely to make things even worse.
a) Male
b) Female
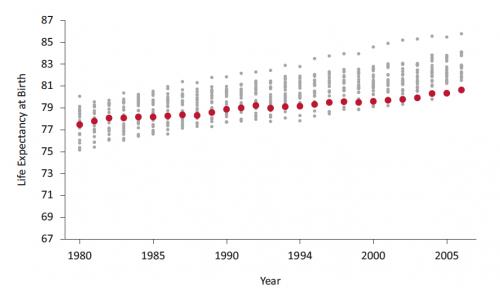
Figure 1. Male (a) and female (b) US life expectancy (red dots), 1980–2006, compared with life expectancy in Australia, Austria, Belgium, Canada, Denmark, Finland, France, Iceland, Ireland, Italy, Japan, Luxembourg, the Netherlands, New Zealand, Norway, Portugal, Spain, Sweden, Switzerland, the United Kingdom and West Germany (grey dots). Taken from the National Research Council/Institute of Medicine (NRC/IOM) report Shorter Lives, Poorer Health
Fortunately, the authors did identify a plus side for US citizens, specifically: “Higher survival after age 75...higher rates of cancer screening and survival, better control of blood pressure and cholesterol levels, lower stroke mortality, lower rates of current smoking, and higher average household income. In addition, U.S. suicide rates do not exceed the international average”.
So what’s the problem?
The authors have put considerable effort into trying to analyse the reasons for the US health disadvantage. They identified problems with the healthcare system itself – fragmentation, limited public health and primary care resources and a large uninsured population – along with individual behaviours and, “The physical and social environment in US communities”. The latter includes such factors as towns and cities being built for vehicles instead of people, thereby discouraging physical activity, and the influence of industry, marketing and other factors on food choices.
Tinkering at the edges
As solutions, the report proposes more comprehensive and better-coordinated research, along with a national public conversation about the issues and urgent efforts to implement policies such as Healthy People 2020 and the recommendations of the National Prevention Council.
So, in a nutshell, while the NRC/IOM report is admirably forthright about the poor outcomes of the US healthcare system, its solutions amount to more of the same and more power for the government and healthcare system. For example, the Dietary Guidelines for Americans mentioned in the National Prevention Strategy currently amount to the MyPlate recommendations – which are themselves part of the problem, rather than part of the solution. And while it would be wonderful if the US could implement the physical activity goals of Healthy People 2020 or the National Prevention Strategy, it’s hard to see how such an almighty turnaround might occur, all things being equal.
Important factors overlooked
But there are even more elephants in this particular room. For one, the US is the society most thoroughly penetrated by genetically modified (GM) foods and their litany of documented adverse health effects. The NRC/IOM, for example, makes no mention of the environmental chemical, ‘electrosmog’ or GM burden to which US citizens are being exposed. There may be insufficient data, but there are plenty of plausible mechanisms, especially when such factors are considered together. And nowhere does the report even consider that the current model upon which the US healthcare system is built might be fundamentally flawed, despite correctly prescribed pharmaceutical drugs being one of the leading causes of death.
Improving health outcomes – naturally
Problems of poor health outcomes associated with national health systems and orthodox medical interventions are not limited to the USA. For us, a rational healthcare system – one based on addressing genuine needs and creating useful jobs – would be based on the following principles:
- Health promotion/disease prevention achieved through diet and lifestyle education, encouraging people to take control of their own health
- Nature-based therapies as first-line interventions to restore homeostasis when problems occur, using nutritional, herbal and other modalities that work with the body’s innate healing capacity
- Reserve the use of new-to-nature drugs, if they are required at all, as well as surgery primarily for emergency situations
- A radical restructuring of the medical curriculum to emphasise prevention, and of hospitals to change from houses of sickness to ‘wellness centres’
- Thorough risk–benefit evaluation of all interventions, regardless of modality – this being something of a specialism at the ANH!
- Integration of insights from the systems biology approach to genetics and nutrition
- Increased use of functional testing of health and wellbeing to provide objective markers of health status and resilience
- A cultural ethos of whole-body healthcare, rather than the reliance on specialised and compartmentalised healthcare delivery as is the norm in contemporary Western healthcare
- A focus on sustainability at all levels of the healthcare system, including in terms of its impact on the natural environment
It’s your call
The NRC/IOM report has one clear message for US citizens: live an average American lifestyle and eat an average American diet, and your health outcomes will be somewhere near the bottom of the pile of industrialised countries.
Conversely, doing things relatively few Americans do will greatly improve your chances of a long, healthy life. Here’s our top 6 tips, all of them backed by solid evidence!
- Don’t smoke
- Minimise alcohol consumption
- Eat plenty of fresh, unprocessed fruit and vegetables
- Engage in 6–12 hours’ moderate to intense physical activity each week
- Avoid taking medications if you can adjust your diet and lifestyle to resolve a health problem. Seek guidance from a qualified and experienced nutritional, functional medicine, naturopathic or other integrative practitioner if required
- Take responsibility for your own health. Don’t hand this power to someone else – it could kill you!








Comments
your voice counts
27 February 2013 at 9:28 pm
Keeping the American Citizen healthy is not what it's about, it's about making them as sick as possible, the authorities are no doubt proud of the poor outcomes, as that is what they want. The less people there are in the world the better. That's what it's about.
28 February 2013 at 10:46 pm
It baffles me how in the face of so much evidence people I know ignore the warnings against RBST in milk,GMO's, chemical laden foods, antibiotic contaminated red meat and poultry. They make absolutely no effort to avoid these things no matter what evidence I present. These are supposedly educated intelligent folks. Is it that they are too busy to do the research for themselves? Is it the barrage of advertising brainwash showing all the pleasing effects of these products and none of the research to the contrary and an assumption that the FDA protects them from harm? My solution is side by side advertising showing the not so pretty side of Doritos for example while advertising a healthful alternitive such as a bean based chip or organic chip. The brainwash has to work both ways so the consumer has honest facts at hand to make purchasing decisions. The information must start to flow in both directions not just the way of the multinational food giants as it exists now. Information and knowledge represent power. The playing field is not currently even.In order for exposure the benefits of good for you products to compete with the money of the cheap highly profitable junk, advertising dollars must go where the competetion is. My belief is that good people will make good choices if exposed to them.
Your voice counts
We welcome your comments and are very interested in your point of view, but we ask that you keep them relevant to the article, that they be civil and without commercial links. All comments are moderated prior to being published. We reserve the right to edit or not publish comments that we consider abusive or offensive.
There is extra content here from a third party provider. You will be unable to see this content unless you agree to allow Content Cookies. Cookie Preferences