Content Sections
Some issues can’t be solved just by throwing money at them. One such issue is the GP crisis in the UK where around 150 GPs are quitting every month. Low morale and early retirement, coupled with insufficient GP recruitment by the UK Government, are forcing the UK’s healthcare system to its knees.
The British Medical Association (BMA) believes that Brexit might worsen the crisis further with “with almost half of the 10,000 EEA [European Economic Area] doctors working in the NHS considering leaving the UK because of the referendum result”. That is, unless the crisis is resolved. But does the Government plan, outlined in the GP Forward View report released last year, that includes increasing funding into primary care by £2.4 billion pa from 2020, really have what it takes to fix the problem? And if you feel like a laugh, check out what Essex GP Dr Tony Copperfield says about the GP Forward View being regarded as "world leading"...
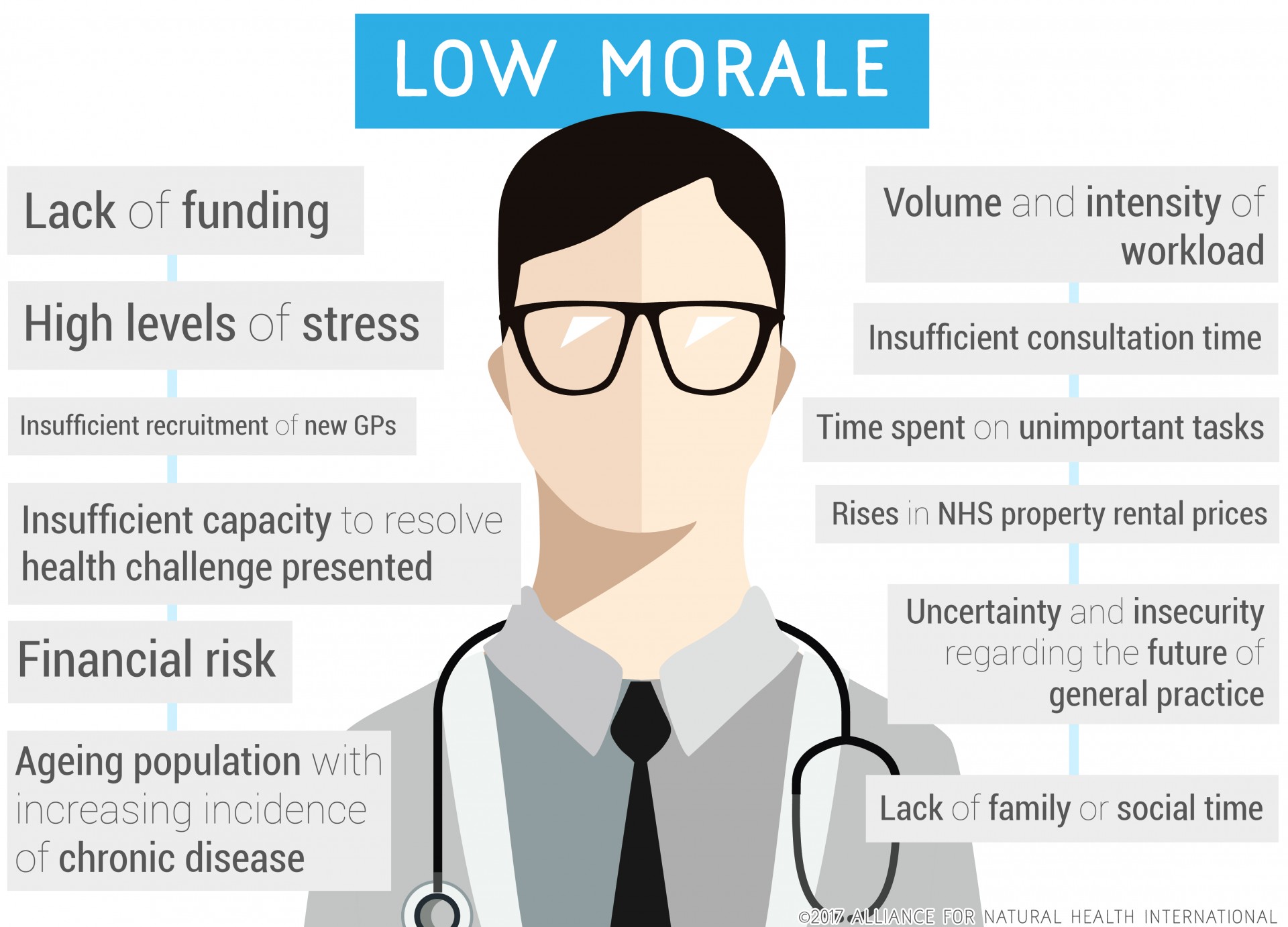
Why GPs are leaving the NHS
The following infographic shows the main reasons why GPs are leaving the NHS at a rate of around 150 per month. It seems that the “jewel in the crown of the NHS”, described as such by none other than Jeremy Hunt, Secretary of State for Health, as recently as 2015, is fast fading.
 Sources [see end of article].
Sources [see end of article].
A big part of the solution
Throwing money at GPs may address some of the issues. But, ultimately it depends what the money is spent on. Nowhere in any of the plans is there any real attempt to provide fundamental reform to deal with the embedded flaw in the delivery of orthodox medicine at the primary care level, which still centrally revolves around diagnosis of a condition and treatment of symptoms with pharmaceutical drugs. These problems are far from limited to the UK – they are a global phenomenon linked to the Western healthcare delivery model.
Among the changes that are needed are the following:
- Disease prevention. Implementation of effective chronic disease prevention strategies that empower and motivate the public to take individual responsibility for health
- Treat early in the disease cycle. Applying effective treatment strategies with minimum risk of adverse effects at the earliest possible point in the disease cycle. These treatments are most likely to involve dietary and lifestyle modification given their effectiveness and safety profiles.
- Motivate and empower the public. Creating and delivering tools and motivators that help empower individuals to take responsibility for their own health and to maximise the effectiveness of self-care.
- Change the medical curriculum. Evidence-informed modification of the medical curriculum for primary care physicians to include pre-clinical disease diagnosis and treatment strategies to significantly reduce the incidence of commonly encountered diseases.
- Reframe health authority advice. Presently Government advice on healthy eating does not align closely with the available evidence, such as in relation to carbohydrate and dietary fat advice. There are also many elements of information missing from advice, such as the creation of harmful compounds (e.g. polyaromatic hydrocarbons, heterocyclic amines) from certain cooking methods or the risks associated with particular food groups (e.g. processed meats and cancer risk). Public advice needs to be entirely reframed on the basis of known benefits and risks.
There are a multitude of other factors that need changing too, and these will be more fully considered in the White Paper we are presently developing for presentation to the UK Government given the opportunities and challenges presented by Brexit.
The overall approach will have application well beyond the shores of the UK.
Have your say
If you’d like to offer solid, evidence-informed ideas about how the pressure might be taken off the primary care system – either in the UK or anywhere else – please email us at [email protected] with the subject line “GP crisis”. Thank you.
Literature sources for infographic
- NHS England. Building the Workforce – the New Deal for General Practice. January 2015.
- NHS England. General Practice Forward View. April 2016.
- Dale J, Potter R, Owen K, Parsons N, Realpe A, Leach J. Retaining the general practitioner workforce in England: what matters to GPs? A cross-sectional study. BMC Fam Pract. 2015 Oct 16; 16: 140.
- Sansom A, Calitri R, Carter M, Campbell J. Understanding quit decisions in primary care: a qualitative study of older GPs. BMJ Open. 2016 Feb 19; 6(2): e010592.
- British Medical Association. Press Release: BMA warns that fall in GP numbers shows crisis deepening in general practice. 29 March 2017.
- Fletcher E, Abel GA, Anderson R, et al. Quitting patient care and career break intentions among general practitioners in South West England: findings of a census survey of general practitioners. BMJ Open 2017; 7: bmjopen-2017-015853.







Comments
your voice counts
12 April 2017 at 9:04 pm
Perhaps GP's are leaving because they are starting to understand that drug based medicine has failed and more importantly, the general public are starting to understand and are now taking their health into their own hands ? (nature rocks !)
12 April 2017 at 10:54 pm
I'm in total agreement with what you propose but it doesn't go far enough. Most primary care physicians are completely oblivious to the importance of nutrition. A very simple proposal would be for physicians to do a full workup on what people are eating and it's potential impact on their health. It would also be useful to allow for treatments that fall outside of pharmacological interventions. I'm aware that you're talking about evidence based but for the NHS evidence doesn't go beyond drug treatments. An overwhelming number of illnesses are related to nutritional deficiencies as well as exposure to toxins (which includes vaccines). As well, the benefits of many alternative treatments is well known from evidence based research that has been done in those particular fields. One of the key ways that the cost of health is going to drop is by allowing for competition across the different types of medicines as well as the use of an authentic evidence based approach that allows for the board that makes decisions on what treatments that are used should have consumer representation and should be free of people connected with pharmaceutical companies. That's why you have treatments such as GcMAF which is excluded for use for cancer as well as a number of diseases in the UK.
13 April 2017 at 7:17 am
The NHS has been talking about primary health care for decades but strangely has done little to put this principle into practice. Their preferred approach seems to be, wait till a patient is really sick and prescribe drugs? Dare we question why this situation exists?
The NHS appears to have a great deal of modern equipment but a GPs surgery usually lack computerised diagnostic programmes and they rely on expensive tests to eliminate possibilities in many cases. Surely Medical Avators, bio resonance machines and other diagnostic options could narrow down possibilities, point doctors in the right direction and save exhaustive testing. This could free up time and money to allow GPs to use their knowledge effectively.
Recently, with a suspected heel spur which makes walking exceedingly painful, I was
advised there was a month's wait for a GP. appointment. A private doctor said she could treat the problem if my GP arranged an X-Ray to confirm the diagnosis. Given my mobility issue I was granted a GP phone consultation.GP.
On requesting an X-ray I was told it wasn't required and what do I expect the doctor to do if the diagnosis was correct ie the doctor seemed to think no further action was needed. When I explained another professional has asked for the X-Ray it was immediately arranged! This reaction seemed to be at odds with the NHS website. The radiologist explained GPs normally do not X-ray or offer treatment for such complaints!
Your voice counts
We welcome your comments and are very interested in your point of view, but we ask that you keep them relevant to the article, that they be civil and without commercial links. All comments are moderated prior to being published. We reserve the right to edit or not publish comments that we consider abusive or offensive.
There is extra content here from a third party provider. You will be unable to see this content unless you agree to allow Content Cookies. Cookie Preferences