Content Sections
- ● From calorie counting…
- ● ….to ‘low carb’ diets
- ● “Avert your gaze from the real problem”
- ● Motor car vs human being
- ● Telling people to eat less doesn’t work
- ● Chicken or egg? Fuel tank size or more efficient engine?
- ● Messed up appetite-regulating hormones
- ● Enter mTOR and AMPK
- ● The 5 magic bullets to reset your metabolic programme
- ● Let’s make it happen…don’t wait for governments to wake up (they probably won’t)
- ● Find some help and a buddy
- ● Dr Rangan did it on BBC!
- ● It’s time to move on
By Robert Verkerk PhD
Founder, executive and scientific director, Alliance for Natural Health International
From calorie counting…
Yesterday the UK government came out with advice telling Brits to eat fewer calories to tackle childhood obesity – if only it were that simple! And haven’t they tried to convince us to consume fewer calories before? If it didn’t work then, why will it work this time around? Anyway, is policy-driven calorie reduction an evidence-based method of dealing with childhood obesity? Doesn’t it encourage people to eat fewer whole foods, cooked from scratch, and more plastic-wrapped, ultra-processed food, replete with a bar code and Nutrition Information panel? They’ve had it wrong almost every time they’ve given us advice, including over the 3 decades they told us to consume low-fat diets!
How to deal with the downstream consequences….?
….to ‘low carb’ diets
That was yesterday. Today the UK government’s nutrition advisory committee has closed its call for scientific evidence on low carb diets. The call was “in response to a request from Public Health England (PHE) in recognition that such diets are increasingly being recommended in the media”.
You see, the media that’s controlled by Big Food, Big Pharma and other Big Companies, now controls the agenda. That’s definitely not science based. But it is certainly politically and economically based. People have heard that low carb diets help them to get their health back. People who’re on low carb diets tend not to eat junk foods given that most are high/refined carb, they eat lots of healthy fats — and they certainly don’t count calories. But clinically we know that these people frequently reverse their type 2 diabetes, they shed unnecessary weight – and they revert to their normal body type quicker than those on any other dietary or drug regime.
We’ve made our submission to the joint Scientific Advisory Committee on Nutrition, NHS England and Diabetes UK earlier today. We found it remarkable that this collection of top scientists and medics have drawn up their inclusion criteria so tightly they’ve managed to find only 12 relevant trials to use as evidence for low carb diets. Come on guys! But then again, we know what they’re doing: despite the raging successes of Banting (Low Carb High Fat) diets supported by restaurants and cafes on the streets of Cape Town, and an increasing number of cities around the world, they’re going to pull down the blinds. Public Health England and its accomplices, let’s face it, are planning to kick low carb into touch, otherwise they would have broadened the inclusion criteria! Anyway, we’re hammering home the point around their scientific myopia. We’ll tell you more when we see what happens as a result of all the consultation inputs.
“Avert your gaze from the real problem”
So – let’s get back to the obesity crisis. Is it as simple as ‘eat less and move more’?
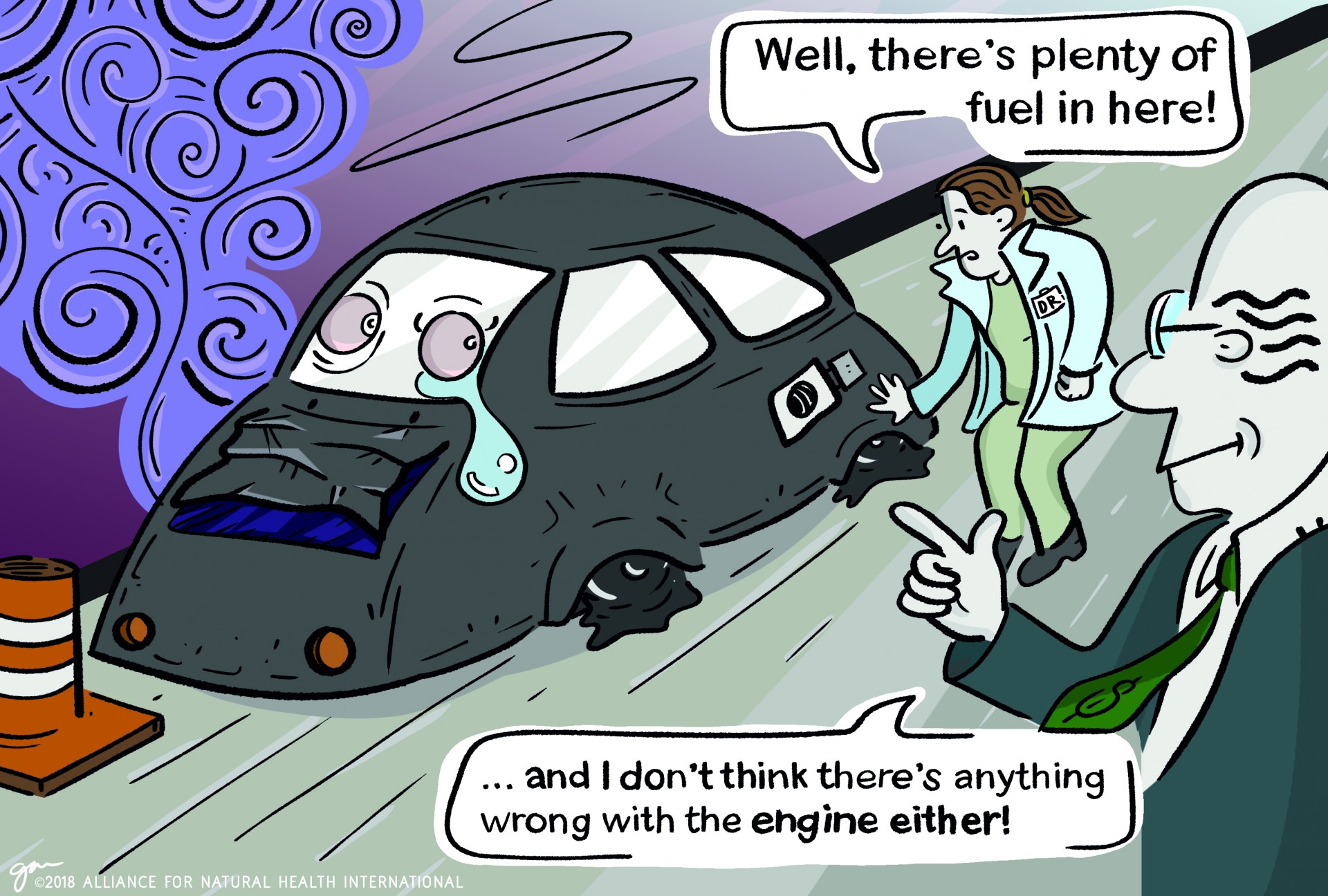
Rather than disappearing into a long scientific discourse on the complex science around obesity, I’ve chosen to simplify our position by way of an analogy. That’s because it’s our view – as well as that of thousands of practitioners and scientists around the world – that health authorities are essentially choosing to look at the wrong part of the problem. Frankly and slightly cynically, it appears likely that they’re doing this deliberately. We say this because we and others have put the science and evidence from both the published literature and from clinical practice in front of them repeatedly and they choose to ignore it. Not once, not twice, but every time. Big Food and Big Pharma have a lot to lose if governments chose to agree with the science and help rid society of these spiralling diseases.
So let’s now try to distill what we consider to be the fundamental flaws of government policy on obesity via this motor car analogy.
Motor car vs human being
It’s definitely easier to think of ways in which humans and cars are different. Cars aren’t living organisms. They’re not sentient beings that rely on conscious and subconscious processes that tell them when and where to fuel. They’re not made from millions of cells, each containing identical genetic material that has all the instructions needed to operate successfully in varying environments. The list goes on. But what about the similarities? They do have the ability to move, they do burn on-board, stored energy, and both have control systems based around feedback loops that govern the efficiency of fuel use in different situations, which might vary anywhere from a whole lot of movement to being idle.
You’ll remember that yesterday, Public Health England told the public it must go on a calorie-counting diet. The health authority wants the public to reduce by 20% the caloric intake of 13 different commercially produced food groups by 2024. That includes pizzas, ready meals, take-aways, sandwiches, savoury snacks, egg products and burgers. That’s like saying, to reduce fuel consumption by cars – and the resultant pollution and climate change effects – let’s force people to put 20% less fuel in their cars at the petrol pump. If you have a 40 litre tank, that means only filling up with 32 litres. It would be a brave person that would argue smaller fuel tanks would be the ticket to reduced fuel consumption and pollution. Wouldn’t most people just fill up more often?
Telling people to eat less doesn’t work
The UK government argues that adults are on average eating 200 to 300 calories more than they need each day. That’s the basis for encouraging a 20% reduction in food intake. As behavioural studies on obesity have shown time and time again, telling people to eat less doesn’t work. Like motor cars with smaller tanks, people tend to either ignore the advice or just ‘fill up’ more often. Seizing on this, Public Health England is also to launch a new campaign that will aim to encourage adults to consume just 400 calories for breakfast and 600 for lunch and dinner respectively, with some so-called ‘healthy snacks’ in between. That’ll work then, D'oh!
For most of us, especially obese people, that’s means going on a crash diet. These calorie reduced diets have a habit of failing spectacularly. What’s most people’s reaction to getting hypoglycaemic, depressed, anxious or just plain hungry between meals? Snacking on some sugar-loaded, nutrient-depleted snack from the nearest fuel station or corner store. What’s more, for most obese people whose satiety and hunger signals are totally scrambled, that’s especially the case.
Chicken or egg? Fuel tank size or more efficient engine?
Let’s get back to the motor car. Environmental and health concerns, as well as unease over the long-term availability of fossil fuels, have forced car manufacturers to make cars both more economical and less polluting. A side effect of this has been that the fuel tanks on many cars have got smaller. They simply don’t need to carry the extra weight of fuel around because of their improved efficiency. The process didn’t start by making fuel tanks smaller. Rather, it involved making changes to the way the car operates, from redesigning the engines, using new, lighter materials, re-mapping fuel injection systems, through to making big improvements in pollution control with the use of catalytic converters.
Now back to humans. What’s really at the heart (pun intended) of the obesity and metabolic disease crisis is a misfunctioning engine, one that asks for fuel when it doesn’t need it, and one that’s forgotten how to burn its most important, long-range fuel, namely fat. In science speak we can refer to the underlying problem driving our metabolic crisis as ‘metabolic dysregulation’. And as you’ll appreciate, if you have a misfunctioning engine, the whole system is affected one way or another. If you want to get back to health, you’re more likely to want to fix your engine than change the size of your fuel tank.
Messed up appetite-regulating hormones
So, what’s wrong with the engine? Our metabolic system is controlled by signalling compounds we call hormones. They work together through a complex system of feedback loops to make up our endocrine (or hormonal) system. A number of appetite-regulating hormones are critical not only to our control of hunger and satiety (feeling of fullness), but also to how we store energy and burn fat. Among the most important are leptin, the ‘energy balance hormone’, ghrelin, the ‘hunger hormone’, and adiponectin, the ‘fat-burning hormone’. Layered on top of this hormonal control of our feeding behaviour and energy use are environmental factors. These include things like our access to food, the nature and properties of the food, and a range of social and cultural norms and pressures.
The science indicates clearly that most obese people show significant cardiometabolic dysregulation, metabolic syndrome and other mortality risk factors – their metabolic engines simply don’t work as nature intended. That’s because our evolutionary history has ensured we’re much better adapted to fasting than we are to feasting. This dysregulated metabolism affects the emotional, cognitive and sensory centres in our brain that control our food intake as well as our desire to exercise. These internal ‘voices’ tend to speak to us much more loudly than any government guidelines or diktats.

The result is that, in obese people, the entire process that regulates feeding, satiation, hunger, physical activity and energy balance in the body is disturbed. Obese people tend to become leptin-resistant and want to continue feeding even when energy stores are ample. Ghrelin triggers hunger when the stomach is empty, being absorbed into the bloodstream. In normal weight people, when the stomach is full and stretched, absorption stops. In obese people who engage in ‘hedonic eating’, ghrelin levels in the bloodstream increase along with specific endocannabinoids, making a person feel hungry even if they’ve eaten recently or have ample fat stores. They get driven to eat, and eat….for pleasure. This state is referred to as ‘hedonic hunger’, it’s particularly common among binge eaters and you won’t find it discussed in government advice.
Baseline adiponectin levels of obese people also tend to be lower than normal-weight people. That reduces the ability of obese people to burn fat, our cleanest burning fuel. There are of course a rash of other signalling compounds that control how we store and use energy, most having somewhat obtuse names such as glucagon-like peptide 1 (GLP-1), cholecystokinin (CCK), peptide YY (PYY) and pancreatic polypeptide (PP). We also see major disarray in the gut microbiome of obese individuals – again something that can be fixed through changes in diets and, for those who can get over the ‘yuk’ factor, faecal microbiota transplantation (FMT).
Enter mTOR and AMPK
There’s a whole other layer of metabolic control that goes on via a system of nutrient-sensing enzymes that have the ability to modify proteins in the body. They’re called protein kinases. There are two super-networks of nutrient-sensing protein kinases that are particularly sensitive to insulin, glucose and essential nutrients. These networks are abbreviated to the scary sounding acronyms, mTOR and AMPK. They control a very wide range of physiological processes from cell growth and energy, protein synthesis, blood glucose, immune function - and much more - as well as helping to regulate metabolism. In people with metabolic diseases like obesity and type 2 diabetes, these systems become deranged. In sedentary, overweight and obese people who snack often and rarely fast for more than 2 or 3 hours during the day, these networks go seriously out of whack. That’s why it’s high time governments started looking not only at food composition and energy, but also at eating frequency.
The 5 magic bullets to reset your metabolic programme
To sort these dysfunctional systems out, telling people to eat 20% less calories isn’t going to cut it. People with metabolic diseases need to reset the control systems of their metabolism within their own engines. And to do that, science and practice tells us we need to do at least five things, all of which are as natural to us as life itself, and all of which have been studied and written about extensively in recent years. They are:
- Caloric restriction – in line with body size and energy expenditure, meaning a one-size-fits-all, 400-600-600 kcal formula is next to useless. Allowing yourself to ‘go hungry’ for increasing periods while being overseen by a practitioner or health coach who specialises in personalised keto-adaption is of course quite a different thing.
- Intermittent fasting – including at least 12 hour overnight fasts and fasting periods between meals of at least 5 hours
- Low carbohydrate/high fat diets – for most people carbs shouldn’t exceed 25% of total energy needs, with healthy fats delivering around 60% and protein the remainder.
- Regular, daily physical activity – including limited high intensity exercise
- Stress transformation – this means getting the best out of your sleep, making time to de-stress and turning negative stress into positive stress.
Public Health England is tackling just one of these – and then, it’s doing it in a way that has been proven not to work. A combination of these four approaches, delivered together using a personalised approach, does something quite profound to the workings of the vast majority of people’s metabolism: it helps those who are on the journey towards full-blown metabolic disease – or in some cases, those who’ve already arrived – to revert to their evolutionary norm. Muscles become stronger, the density and volume of energy-producing mitochondria in them increasing greatly. This evolutionary norm means being what is called ‘fat-adapted’ or ‘keto-adapted’. In a nutshell, that’s a state in which the body is able to function in ‘nutritional ketosis’ where it can readily burn fat in the absence of carbohydrates, generate ketones in the liver in the process and use them as fuel in our mitochondria. This is our evolutionary system that allows us to have sufficient endurance to go without food for days and still have sufficient energy to find it. With fridges, supermarkets, corner stores and fuel stations all around us – many of us have allowed this system to go dormant. The level of ketone bodies in the blood of healthy, keto-adapted individuals who are in nutritional ketosis is low (0.5-3.0 mmol/L), well below those levels associated with diabetic ketoacidosis or starvation.
Left to right: Drs Jeff Volek, Steve Phinney and Tim Noakes – the modern day fathers of LCHF diets
Being keto-adapted doesn’t of course mean you can only burn fat – but it does mean you’re metabolically flexible and resilient which is your best possible insurance against chronic and degenerative diseases. Once enough people, hopefully including some health authorities, some members of the medical profession – but most of all the public – recognise that becoming keto-adapted and metabolically flexible deals with the underlying causes that link obesity, heart disease, type 2 diabetes, Alzheimer’s and other metabolic diseases together – it will be game over. The biggest burden on our healthcare systems will be gone. The only losers will be Big Food and Big Pharma. Big Food specialises in producing high carb, ultra-processed foods that titillate cross-talk between opioid and cannabinoid receptors in our brains. Big Pharma sells truckloads of lipid lowering and blood sugar regulating drugs that do little or nothing to deal with the underlying causes of the metabolic dysfunction brought on by our contemporary, screen-filled, technology-laden lives. How many fewer of us will have need for Big Food and Big Pharma's products?
Let’s make it happen…don’t wait for governments to wake up (they probably won’t)
So how can we make it happen? To do all of this, we need a fundamental re-structuring of governmental and medical advice for obese, type 2 diabetic, prediabetic and other metabolically diseased individuals. We need healthcare and fitness professionals to understand and engage with the underlying science and work together to support people on their journeys. We need peer-to-peer support, guided by ‘keto health coaches’. We need individuals to supplement with additional peptides, amino acids, fats and a host of different micronutrients and plant compounds that can help correct the dysregulated metabolism. Yet governments are continuously erecting regulatory hurdles to make access to natural products – and especially communications about them – more and more difficult.
Governments don’t appear to be interested in looking at the right part of the problem. They seem content to focus their gaze on the fuel tank while telling us to put in less fuel. They appear set on ignoring the misfunctioning engines within so many of our bodies in the hope we won’t wake up to their real mission. That’s more about the corporatocracy making money out of addicted and diseased citizens than it is about helping them deal with the underlying metabolic dysregulation caused by 21st century, ultra-processed, industrial lifestyles.
Find some help and a buddy
But let’s end on some good news. There’s a band of healthcare practitioners and coaches out there who understand this stuff – and who know how to fix it. Some, but presently very few, are medical doctors. Many more are functional medicine practitioners. Others practice under the banners of integrative medicine, lifestyle medicine, or Clinical Psycho Neuro Immunology. When you’re looking for a practitioner or health coach, you specifically want to ensure that one of their specialities relates to supporting keto-adaption.
It’s also worth mentioning that there are other groups of practitioners whose advice could push you in the opposite direction to where you want to go metabolically – even deeper into disease. High on the list here are most (but fortunately not all!) registered dieticians, given their continued desire to feed us inappropriate foods, little and often, in ways that we know push people ever deeper into ‘diabesity’.
Dr Rangan did it on BBC!
Strangely – despite Dr Rangan Chatterjee showing 6 million UK viewers how to do it on primetime television with his Doctor in the House series on BBC One, functional medicine practitioners have yet to be invited onto government advisory panels. Given the urgency of the matter, when will health authorities wake up and realise they should be talking to clinicians who’re routinely helping people to recalibrate their metabolic engines and to reverse type 2 diabetes and obesity. Being guided by researchers who’re looking at tiny pieces of an artificial picture based on historic clinical trials – while deliberately avoiding looking at the real world around them, isn’t going to fix anything. They need to be talking to the best clinicians in the business of healthcare and find out how they’re doing it. But then again, they don’t want to help people get better, do they?!
British ‘specialist generalist’, functional medicine-trained doctor, Dr Rangan Chatterjee
It’s time to move on
So let’s just get on with it! There’s no point waiting for government authorities or the mainstream medical profession to tell us what to do. Most of the real work in reversing obesity and metabolic disease is being driven by the grassroots, not the medical profession. Doctors are seeking training, because they’re being asked about it by their patients!
The mainstream medical establishment and government health authorities may or may not come on board. Their track record doesn’t stand up to much. Perhaps their best skill has been to help an increasingly large sector of the population become ill and dependent on a mainstream healthcare system that can do little to help them.
For an abbreviated version of this article, go to the HealthInsightsUK website operated by leading UK health journalist Jerome Burne.
To help disseminate the views expressed above, please feel free to publish this piece in full via any printed or electronic media on the condition that:
- publication is notified to ANH-Intl (please email [email protected]) prior to publication.
- acknowledgement is made both of the source www.anhinternational.org and author (Robert Verkerk).











Comments
your voice counts
08 March 2018 at 2:21 pm
Thanks for this; you have articulately summarised observations I have been making about our health systems, governments, Big Food and Big Pharma, for years. With so many of us being convinced by these powerful institutions, that very unhealthy choices are the way to some kind of 'health', one can feel somewhat out on a limb when common sense and personal observation tells us that most conventional dietary and health advice is likely to do more harm than good.
Your voice counts
We welcome your comments and are very interested in your point of view, but we ask that you keep them relevant to the article, that they be civil and without commercial links. All comments are moderated prior to being published. We reserve the right to edit or not publish comments that we consider abusive or offensive.
There is extra content here from a third party provider. You will be unable to see this content unless you agree to allow Content Cookies. Cookie Preferences