Content Sections
Biomedical blind acceptance
The dominant biomedical (Western) model of healthcare suggests that health problems are the result of failures of biology, hygiene or behaviour. Implicit or explicit is that these health problems require delivery of biomedical treatments – pharmaceuticals, and that delivery is mainly by physicians or other healthcare providers.
This model has been the primary reason why the richer a country, the more money it tends to spend on both health professionals and pharmaceuticals.
But very few studies that have attempted to link specific aspects of the biomedical model – that has enjoyed spectacular growth during the post-WWII period – with population health.
That’s why a study just published in the Journal of Health and Social Behavior by two health sociologists, Hui Zheng from Ohio State University and Linda George from Duke University in North Carolina, is of such interest.
New study – using OECD data
The study’s main focus has been to evaluate underlying mechanisms for a widely accepted theory, epidemiologic transition theory, based on the work of Omran in 1971, that upholds that human development transitions through 3 stages of development. The first stage is the age of pestilence and infectious disease that characterised most of human history, then to receding pandemics in the middle of the 1800s in the developed world, through to advancing age of degenerative and human-created disease (especially cardiovascular disease) in the early 1900s.
In 1986, Olshanky & Ault modified the theory, adding a fourth stage, which is representative of the most technologically advanced and richest societies. This stage is reflected when mortality rates from degenerative diseases, notably heart disease, stroke and cancer, undergo major and unexpected declines.
There is broad acceptance in different societies – and certainly in politics – that this fourth stage of epidemiological transition has been associated with the development of Western medicine and pharmaceutical drugs - the two generally being viewed as intimately associated.
However, in the absence of proof of this mechanism, a number of other theories have persisted, including the conflicting theory of McKeown and colleagues from the mid-‘70s which argues that broad socioeconomic conditions, most notably diet and nutrition, are the root causes of improved population health throughout history, not medical progress.
The Ohio University study looks at three key components of the biomedical model. These are: 1) investment in medical infrastructure, 2) the size and specialisation of the medical workforce, and 3) the size of the pharmaceutical industry. All of the data used in the analysis are derived from a 26 year period (1981-2007) and are sourced from the Organisation for Economic and Co-operation and Development (OECD)).
Study take-homes
Based on these OECD data, the main take-homes from the study are:
- The first two of these factors, in other words healthcare expenditure by a country, and the size and degree of specialisation of the medical workforce, were unsurprisingly found to be positively correlated with health outcomes
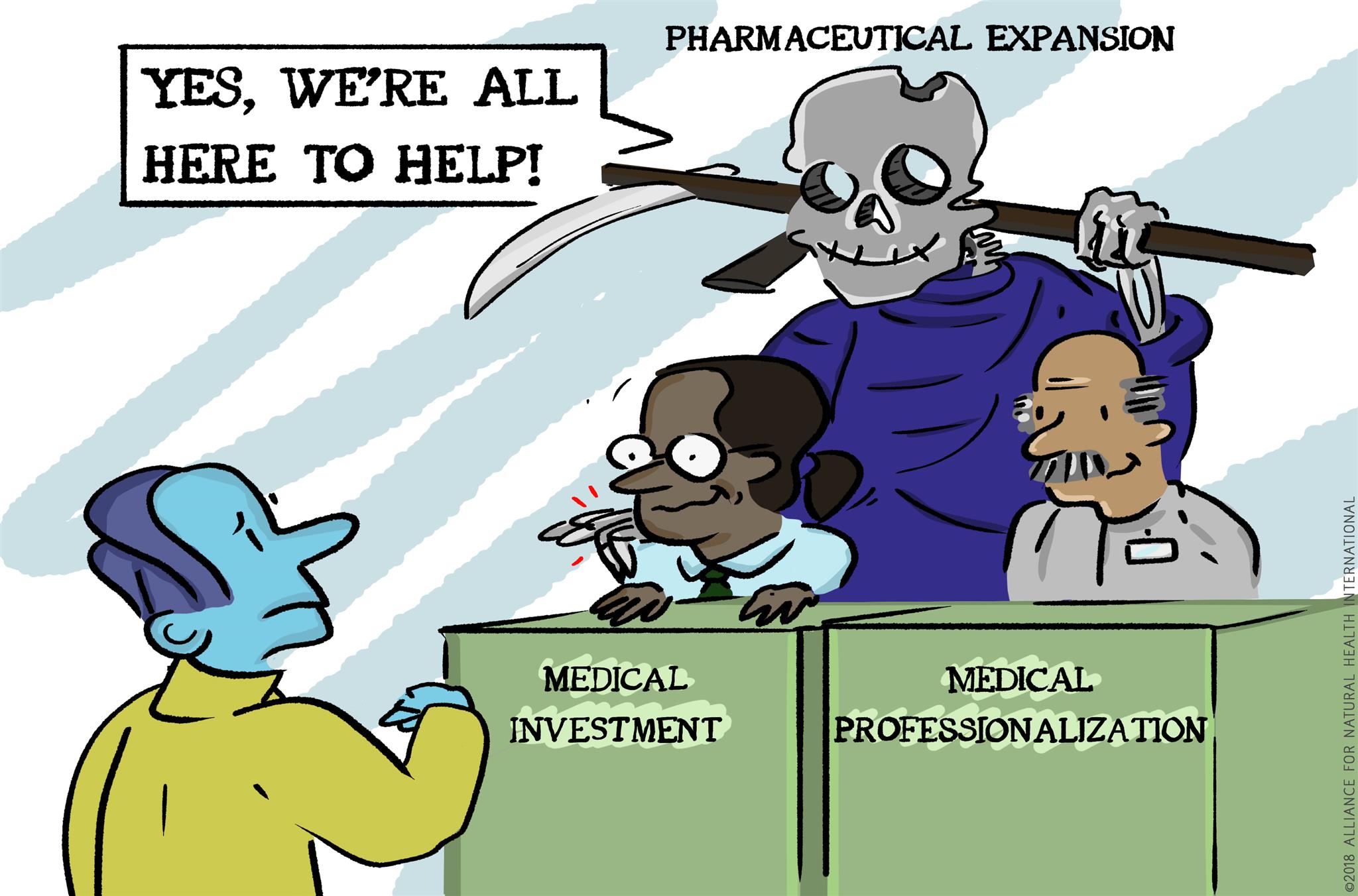
- More surprising was that the third component, the size of the pharmaceutical industry, did not correlate consistently with improved health outcomes. In fact, the the scale of the pharmaceutical industry had a particularly negative impact on health outcomes in older women (over the age of 65)
- And finally, the more the pharmaceutical industry expands in a given country, the more it appears to negatively impact the beneficial effect of medical professionalisation and specialisation. Pharmaceuticals therefore appear to compromise the effects of doctors and specialists, rather than facilitating better outcomes.
So what?
In essence these findings drive a coach and horses through conventional wisdom that suggests that it is the combined effect of more drugs and more doctors and specialists, that delivers better health outcomes. That's why as countries get richer, they spend more money on healthcare providers as well as spending more money on drugs. But it is the drugs themselves - generally posited as the key part of most doctors' intervention – that are the 'fly in the ointment'.
The findings shine more light on McKeown's theory from the mid-1970s that it's not medical progress, but more money in the hands of consumers that causes them to consume better diets and have healthier lifestyles, that are the main drivers of better health outcomes.
This study is incredibly timely, as it entirely supports some of the underlying premises in our own position paper on health system sustainability in the UK that’s going out for consultation along with an invitation to endorse the final version during the week beginning 9 April.
If you live in the UK or you’re interested in being involved in the consultation, or might be interested in endorsing the document to give it more political weight, please email the ANH team at [email protected] and include ‘SHS consultation’ in the subject line.
Let us know your organisation or your registration body. We’ll make sure you receive by email during the week commencing 9 April the draft position paper, along with a short guideline document.








Comments
your voice counts
28 March 2018 at 10:09 pm
Interesting title, but don't the doctors prescribe the drugs that do kill ?
I understand that most doctors now understand that the drugs they prescribe for chronic diseases, are harmful and that nature provides superior treatment for all chronic diseases, yet they are obliged to follow this treatment regimen or lose their licences to practice ?
29 March 2018 at 12:39 pm
In essence you are right, although most doctors do not have adequate training to deliver effective non-pharmaceutical protocols. This expertise exists among health professionals who have been marginalised by the mainstream medical establishment. If, as a society, we're going to be serious about our efforts in resolving some of the NHS's woes, most of which are caused by excessive burden from comorbidities for which effective, NICE-approved protocols are sadly few and far between - it's time to invite these health and fitness professionals back to the table. Best wishes, Rob
29 March 2018 at 12:07 am
Wonderful to read this. Thank you. For too long we have been indoctrinated with the myth that we all live to greater ages because we pop Benzodiazapines, Opioids and Statins etc. The real truth is, we live longer largely because of plumbers and thanks to industrialisation we have enough food, water, shelter, shorter working hours, better sanitation and protection from the dangers in the wild. I often wonder if the net benefit of the great things medicine can do is totally negated by the damage of new to nature synthetic chemicals being relentlessly pumped into the natural environment of the human body
29 March 2018 at 12:28 pm
Hi Paul - the OECD data would tend to suggest this: that the benefits of good doctoring are increasingly negated when doctors become over-reliant on drugs as their key tools. The idea that drugs and vaccines are inseparable from good healthcare is something society has bought lock stock and barrel without much in the way of supporting evidence. Hopefully things are changing...Best, Rob
29 March 2018 at 11:25 am
I read your article in "What Doctors don't Tell you" every month, I also believe in preventing ill health by eating a healthy diet and exercising, I'm in my seventies now, work in my business six days a week, do not eat takeaways or fast food, walk and climb stairs regularly. I take no medication except an Inhaler for my asthma which I probably got from our polluted air in London, I firmly believe the less medicines we take the better and am very glad that you are spreading the word, long may you continue!
29 March 2018 at 11:44 am
Dear Isolde - you are a perfect example of someone who's doing so many things right and reaping the benefits. Hopefully you're able to help others around you to do as you do! London air is a problem for everyone, but lots of house plants indoors, walking as far away from busy roads as possible, and keeping lots of plant nutrients in your diets (a rainbow every day!) all help. We do what we can to keep spreading the word - and all of us benefit from people like you doing the same! Best wishes, Rob
30 March 2018 at 11:37 pm
Ah, I fully agree with you, but even though I have ticked all the boxes for the past decade, I had an MI out of the blue two months ago! I left hospital 5 days later with a goody bag full of medications for the rest of my life. I refused the statins, but was prevailed upon to take the aspirin, anti platelet aggregation med and a beta blocker. As my diet is chock full of natural anti platelet foods and supplements, I question further medication, and my life has been made most unpleasant by the collateral damage on my neck and shoulders by the beta blocker. Nobody wishes to tailor the meds to my lifestyle, which is radically different from the vast majority of the population. I was so proud of myself, having reached my seventies without major illness or pharmaceuticals.
31 March 2018 at 2:26 pm
Alas, I have not been as lucky as Isolde. Despite having ticked all the boxes for the past decade, I suffered an MI in January. I was presented with a goody bag of pharmaceuticals as I left hospital five days later. I refused statins, not only on principle, but because my cholesterol level is good and I have no occlusion, but was persuaded that it was imperative for me to take an anti platelet med, aspirin and a beta blocker. The net result is that the collateral damage from the meds is making my life unpleasant. I hold that my lifestyle and diet are so radically different from the norm that the quality of care meds are not necessarily appropriate. Getting a GP to accept this fact is well nigh impossible!
Your voice counts
We welcome your comments and are very interested in your point of view, but we ask that you keep them relevant to the article, that they be civil and without commercial links. All comments are moderated prior to being published. We reserve the right to edit or not publish comments that we consider abusive or offensive.
There is extra content here from a third party provider. You will be unable to see this content unless you agree to allow Content Cookies. Cookie Preferences