Content Sections
By Rob Verkerk PhD, founder, executive and scientific director, ANH-Intl
Heard the news? It’s been doing the rounds of the big media channels for the last week or so. The message screaming from the headlines has been to the effect: “VITAMINS DON’T WORK”. Sometimes the articles go one step further and add a tag line that alludes …”AND THEY MIGHT EVEN KILL YOU”. It’s of course not new news for most of us – we’ve heard it all before. Many times.
Here’s a small selection of what’s been circulating:
Independent, “Vitamin and mineral supplements offer no health benefits, study suggests” (5 June)
The Guardian, “Vitamins and antioxidants: some supplements linked to increased risk of death” (28 May 2018)
Forbes, “Aside From Folate, Vitamins Appear Largely Ineffective For Prevention, Study Finds” (28 May 2018)
Newsweek, “Do vitamin and mineral pills actually work? No, say scientists” (29 May 2018)

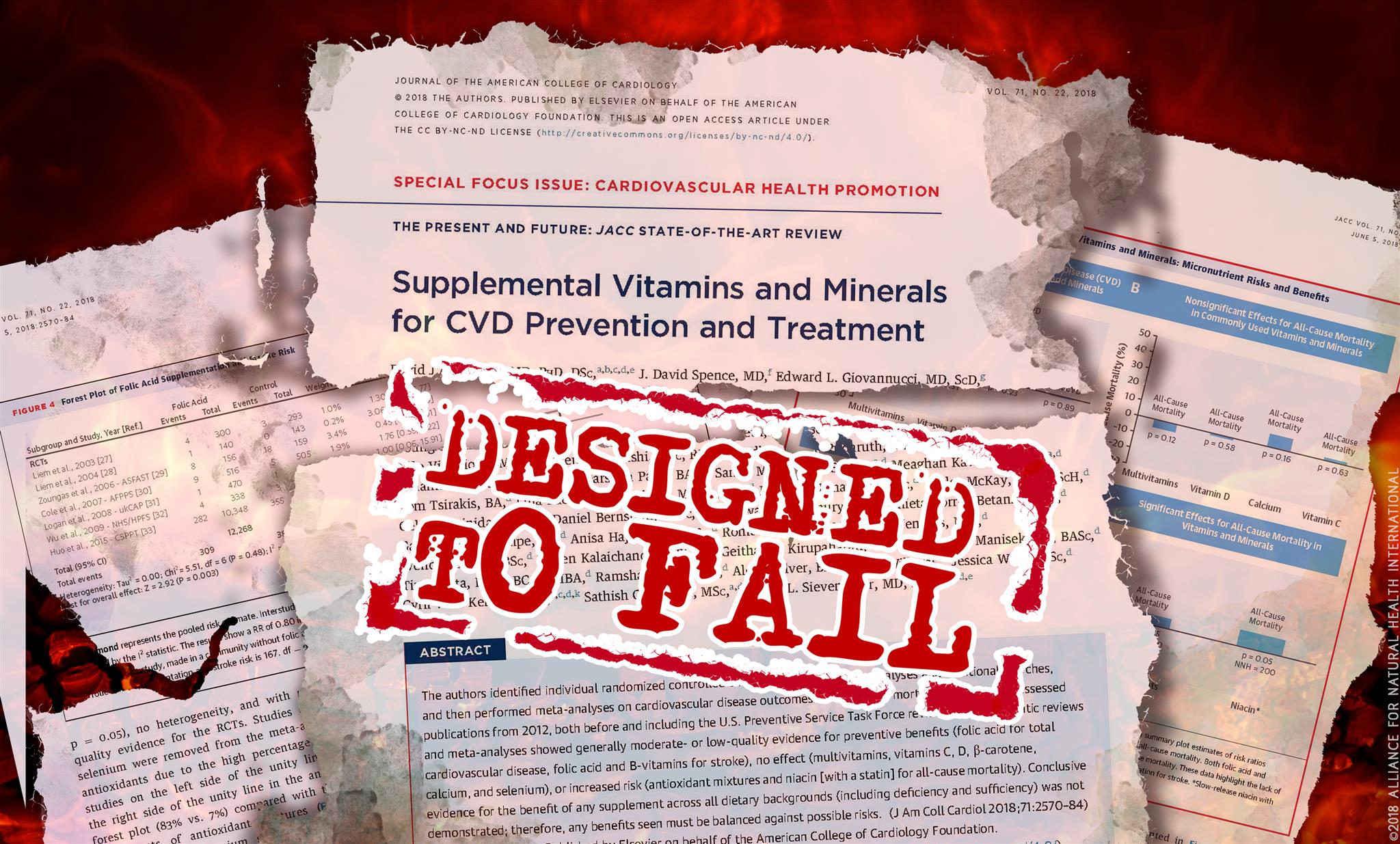
The ‘not-so-new’ study
The trigger for all this news wasn’t a new vitamin study, but rather a new study of studies, a new meta-analysis, investigating the link between multivitamin, single- or paired-vitamin supplements and cardiovascular disease (CVD) risk and death. The meta-analysis included 179 old (pre-2012) studies and only 15 studies since this time. It was published in the Journal of the American College of Cardiology which is considered the leading peer-reviewed heart disease journal in the world. In effect, the results of this study will be seen by a very high proportion of cardiovascular specialists around the world, and certainly all of the most influential.
These studies are part of the work of the U.S. Preventive Services Task Force (USPSTF) recommendations on vitamin supplements to prevent cardiovascular disease.
It follows a previous meta-analysis that pointed to inconclusive findings between the balance between benefits and harms.
Why the study fails
Any health authority that's serious about prevention needs to ask the question: what’s the best advice we can offer the public that will prevent or limit chronic, preventable diseases, in this case CVD. When it comes to supplements, that would be appropriate alongside a balanced and varied diet, ample physical activity, healthy stress reduction and transformation practices – no clinician worth his or her salt would be recommending a multi or a very limited combination of synthetic nutrients.
The star-studded, 39-strong team of authors led by leading nutritional scientist Professor David Jenkins (who pioneered the glycaemic index), would certainly give the impression of a consensus view. Apart from Jenkins, himself a strong advocate of plant-based diets for reduced heart disease risk, amongst the authorship is none other than Reinhold Vieth, one of the most well-known advocates of high-dose vitamin D. Unfortunately, neither plant-based diets nor high dose vitamin D make any kind of an appearance in the meta-analysis.
The declaration of interests of the authors also make interesting reading. In fact, it’s rare to see so many declared. Interests in the following companies are declared: Kellogg’s Company, Quaker Oats, Procter & Gamble Technical Centre Ltd., Bayer Consumer Care, Pepsi/Quaker, Soy Foods Association of North America, the Coca-Cola Company, the Canola and Flax Councils of Canada, Barilla, Unilever, Unico, Primo, Loblaw Companies, Quaker (Pepsico), Danone, Bayer Consumer Care and DuPont Nutrition and Health.
On ‘the other side’, you’ll find declarations linked to Better Therapeutics (FareWell), Verywell, True Health Initiative, Institute of Food Technologists, Saskatchewan Pulse Growers, Sanitarium Company, the International Tree Nut Council Nutrition Research and Education Foundation, Herbalife International, Pacific Health Laboratories, Nutritional Fundamental for Health, Metagenics and the Canadian College of Naturopathic Medicine. Some would see this as a balance of interests, but as we’ve seen before, the weight of ‘Big Corporate’ has shown great capacity to drown out the voices of smaller companies.
That’s why we argue that the fundamental tenet of the study does a disservice to public health. This is further evidence of how research funds are wasted needlessly – delivering results that were entirely predictable and of little value to the public.
Top-line concerns
- The questions the meta-analysis sought to answer were ones highly likely to yield negative results i.e. does a simple multivitamin, such as Pfizer’s Centrum Silver® product used in the Physician’s Health Study II, reduce cardiovascular disease (CVD) risk or risk of death? It seems unlikely given what is already known from previous studies using these kinds of synthetically-derived vitamins, although it’s noteworthy they have been shown to produce a modest, and statistically significant reduction in cancer in older, male physicians. Frankly, the public seems to be more aware of the likely benefit of multivitamins than do the researchers; we’ve yet to meet a single person who believes a supermarket or pharmacy ‘multi’ is a useful insurance policy for heart disease. Interestingly, a survey by DSM, now the largest maker of vitamin and mineral raw materials used in supplements, showed that most people take their ‘one-a-day’ multis for general health or for filling a perceived nutritional gap in their diet.
- In contrast to popular reporting of the study, the results weren’t entirely negative. The meta-analysis found benefits especially on stroke from folic acid and other B vitamins, this being driven especially by a large, 5-year Chinese study where there was no background folic acid fortification. Had the 20% reduction in risk of stroke found for folic acid been found for a drug, Pharma companies would have been shouting the result from the rooftops! Putting this in perspective, the number needed to treat (NNT) to protect against one case of stroke was 176, while that for statins found by a meta-analysis carried out by the Cochrane Collaboration (2013) was less favourable at 196.
- The negative results for ‘antioxidant’ studies on all-cause mortality were manipulated by the removal of all studies containing selenium which showed clear benefits. This is unashamed data massage because selenium should be included given it is an antioxidant mineral. This manipulation turned what would have been a positive result to a negative one. Researchers continue to view antioxidants from a very limited perspective (as if vitamins A, C and E are the only antioxidants!) by ignoring the host of botanical antioxidants that in nature (fruits, vegetables, herbs, spices) are associated with the delivery of vitamin and mineral antioxidants.
- The negative result for niacin does not refer to all forms of niacin - only to flush-free niacin forms, and therefore not nicotinic acid (that induces a reversible flush that lessens or disappears once tolerance is achieved). This is an issue I’ve discussed in my 2010 paper in the journal Toxicology.
- There are numerous problems with many of the included studies. One of the most common problems was that supplementation periods were too short or that supplementation was started too late in an individual’s disease cycle. As important, are issues relating to the forms of nutrients (these often being far from optimal and not including the biologically-active or natural food forms), the combinations of nutrients used (often too limited) or dosages of micronutrients (generally too low, occasionally too high for the wrong type of nutrient e.g. synthetic beta-carotene). Additionally, the follow-up periods were often too short and the end-points being monitored (e.g. CV events, death) were far from ideal given the ‘treatments’.
- Meta-analysis of previous studies of older populations at high risk of heart disease is far from the best way of determining the most appropriate supplementation regimens for protecting healthy and younger population groups from the full range of chronic diseases that afflict so many later in life.
- This meta-analysis was unlikely to give a fundamentally different outcome from the previous meta-analysis informing the U.S. Preventive Services Task Force (USPSTF) on recommendations for vitamin and mineral supplements on CVD because only 15 of the 179 studied included were new. But, it did provide another opportunity to generate negative headlines around the world.
Where to from here?
We’re convinced that while meta-analyses can be regarded as powerful tools that combine data from other studies, they are of little use when trying to formulate chronic disease prevention protocols. Much of that’s down to the fact that any meta-analysis is only as good as the data that goes into it. This latest meta-analysis is a classic example of irrelevant data in, irrelevant data out. In some cases, it’s actually trash in, trash out. That’s particularly when you’re looking at the many included studies reliant on limited periods of supplementation with less-than-ideal supplement forms or doses.
We see two parallel solutions, and we’re intimately involved with both.
Risk/benefit analysis – using the TNO model
Firstly, there’s a crying need for developing using risk/benefit analysis for understanding optimal supplemental ranges for different groups, rather than just relying on what Pfizer, Bayer or another pharma company think might be reasonable. This has been the starting point for determining the public health advice on the number of portions of oily fish that are optimal, given that too much might incur risk from heavy metals.
The TNO model that we’ve commissioned was published last year. We’re still raising funds to ensure that vitamin B6, vitamin D and some other micronutrients that are being pulled off shop shelves in Europe by over-zealous regulators are analysed in this way. The ‘demo’ cases for folate and iron published alongside the model provide a taster of what the model will deliver: for folate it’s 4100 mcg/day except in vitamin B12-deficient individuals, when it’s 1,100 mcg/day. For iron bisglycinate (‘gentle iron’) it was 69.2 mg/day, while for iron sulphate it was just 13.3 mg/day. Presently, the system being used by regulators the world over relies on applying the risk from the most toxic form of the nutrient to all other forms, irrespective of their safety. So in the case of iron supplements, regulators apply their determination for iron sulphate to all forms of iron, including bisclycinate – something any lawyer will tell you is disproportionate. More than that, it’s an abuse of our fundamental human rights.
‘Big data’ project – the Hawthorn Health Collaboration
The second part of the solution involves looking at ‘big data’ where it’s possible to tease out of the mire those people with the best health trajectories and the lowest disease incidences. These data would allow us to find out what kinds of diets, supplements, lifestyles and healthcare patterns are associated with high levels of health, not just diseased states. As it happens – this is a key goal behind the Hawthorn Health Collaboration.
A final word
Given everything we’ve just discussed, let me clarify a misconception disseminated by the world’s media which I raised at the outset of this article that I now feel compelled to rectify: VITAMINS WORK – WE DIE PREMATURELY IF WE DON’T HAVE THEM IN THE RIGHT FORMS AND AMOUNTS.
However, our individual, genetic and epigenetic differences mean there isn’t a one-size-fits-all vitamin protocol. Balancing micronutrients is fundamental to long-term health as explained by Prof Bruce Ames in his triage hypothesis.
But it needs the right forms and amounts for a given individual – and even that changes over time. Any clinician (and we know hundreds) who has assimilated clinical test results from blood samples over many decades will tell you that intakes many times greater than the RDA or NRV are often needed to normalise circulating levels in the bloodstream. We also know that ‘normalised’ circulating levels of micronutrients and other molecules reflect a body that is in balance. This balance (homeostasis) is a prerequisite for the appropriate function of the myriad signalling systems within our bodies that continually aspire, given the right microenvironment, to an optimal state of health and resilience.
All of this – as any good health practitioner or doctor will tell you – takes more than just popping a daily multi.







Comments
your voice counts
06 June 2018 at 8:23 pm
The basic flaw in all studies is lack of dose response. What is the correct dose? Then freeing us from the vaunted RDA as a non sensical notion.
Meta analyses are also flawed. Frequently measuring only two data points rather than a series of data points. Did the patient achieve sustained therapeutic levels?
Finally always ask what was the intended purpose of the study. There usually is an underlying motive.
BTW, a true absolute vs relative statistical analysis of statin efficacy shows zero benefit population wide. And what about the current flu vaccine with 10% efficacy. So it begs the question what is the efficacy of any therapeutic?
07 June 2018 at 7:49 am
Thank you for taking the time to comment Philip. Good points and very good questions!
Warm Regards
Melissa
07 June 2018 at 2:23 pm
Thanks Philip, agree 100% with all of your views. Hopefully there is a fundamental shift going on re: awareness of the gross inadequacy of most methodologies still currently being used to underpin pharmaceutical dominated evidence-based medicine
Kind regards,
Rob
06 June 2018 at 11:19 pm
Finally, someone said what needed to be said! Too often, misuse and manipulation of statistical data causes the public to be misinformed on prominent issues like these. Thanks for saying ehat neede to be said.
07 June 2018 at 7:52 am
Thanks for your support Joanne.
Warm Regards
Melissa
07 June 2018 at 10:38 am
The upcoming shortfall in public health, particularly children's , will need very serious supplementation if we are not to lose a whole generation.
08 June 2018 at 10:55 am
A multivitamin is not much good for deficiencies.
The required amounts are too weak and add to the fact some vitamins work against each other.
Eg. Vitamin c works blocks vitamin b absorption
In the case of b12 and folate deficiency, low levels can cause high homocysteine. To break down harmful homocysteine levels treatment is by b12, b6 and folic acid. Many cardiologists don’t know anything about high homocysteine which caused narrowing of the arteries.
08 June 2018 at 11:20 am
Awesome article, clear and precise!!😊
08 June 2018 at 7:25 pm
#VitaminsB4Pharmaceuticals
09 June 2018 at 6:44 am
Sound common sense data but where can a individual get help to balance nutrient deficiencies they know they need
09 June 2018 at 12:29 pm
Hello Diana, people can consult with a qualified functional medicine practitioner to get individual help in optimising health and nutrient intakes. You can find a practitioner in your area on the Institute for Functional Medicine's Find a Practitioner page - https://www.ifm.org/find-a-practitioner/.
Warm Regards
Melissa Smith
18 June 2018 at 8:14 am
Great article. It must be said but I wonder if it will make any difference... the mainstream media are so manipulated and controlled that they won't publish any article of this kind.
BTW where do people find information about supplements that are really worth taking?
18 June 2018 at 4:49 pm
Hi Marc
Thanks for your comment. We do keep trying to coax the mainstream media into publishing information on both sides of the debate but it seems that objective journalism may be a thing of the past. It's why we must maintain our freedoms on the Internet at all costs.
You're not the first person to ask about reliable information on supplements. You could look at The Therapeutic Research Center (https://naturalmedicines.therapeuticresearch.com/) or The Natural Medicines Database (http://naturaldatabase.therapeuticresearch.com/home.aspx?cs=&s=ND&AspxAutoDetectCookieSupport=1), which are more related to US supplements, but you can also search for up to date scientific information on ingredients.
However, we would always recommend a 'food-first' approach (see our Food4Health guidelines: https://anhinternational.org/campaign/food4health/) with targeted supplementation that's been individualised for you by a suitably qualified practitioner. One size really doesn't fit all as everyone's needs are so unique.
I'm not sure exactly where you're based, but you might like to take a look at the Institute for Functional Medicine's practitioner link: https://www.ifm.org/find-a-practitioner and see if there is anyone close to you. Alternatively, nutrition practitioners or naturopaths are also well-versed in the use of food supplements. Once you have a list of suggested supplements from a practitioner, it's easier to find current scientific information on the generic ingredients.
Best wishes
Meleni
Your voice counts
We welcome your comments and are very interested in your point of view, but we ask that you keep them relevant to the article, that they be civil and without commercial links. All comments are moderated prior to being published. We reserve the right to edit or not publish comments that we consider abusive or offensive.
There is extra content here from a third party provider. You will be unable to see this content unless you agree to allow Content Cookies. Cookie Preferences