Content Sections
What’s the best diet for a pregnant woman and her unborn child? Are there foods that should be avoided? The Nutrition Society, in the manner of many other organisations and authorities, warns about soft cheeses, raw eggs, fish like swordfish and marlin high in heavy metals, and even vitamin supplements containing vitamin A.
But like most establishment bodies, they don’t hint at any risks linked to the consumption of gluten or grains. Many bodies positively recommend consuming wholegrains as part of a so-called ‘healthy diet’. What’s going to happen now there’s a major study out, published in the British Medical Journal, that says women who eat the most gluten run a two-fold greater risk of giving birth to a child who develops type 1 diabetes compared with those who consume the least.
The study isn’t conclusive because it’s based on a 360 item food frequency questionnaire answered between 1996 and 2002 by over 90,000 Danish women in week 25 of pregnancy. Follow-up was about 15 years. But the proportionate increase in type 1 diabetes incidence in children born to mother’s consuming more than 20 grams of gluten a day, compared with those consuming less than 7 grams per day, was inescapable. This comes at a time when there’s a push to try and cement and increase whole grain consumption internationally, including in Asia where gluten-containing grain consumption has traditionally been “very low”. In trying to explain this robust trend, the authors of the Danish study, led by Julie Antvorskov and Knud Josefsen from the Bartholin Institute in Copenhagen, consider the complex interplay of factors that might be responsible. It includes the pro-inflammatory effects of gluten and its potential to increase gut permeability and elicit autoimmune reactions. They also reference a lot of the published science, both in animal studies and humans, that points to inflammatory, immune and autoimmune effects of gluten in the diet.
The emerging evidence of risks associated with gluten, including on unborn children, is the very reason the ANH Food4Health guide, unlike guidance from governments or most other authorities, avoids all gluten-containing foods. We sometimes find ourselves getting a little impatient about complaints being made by the pro-gluten brigade which so often expresses concern about the risks of key food groups being left out. These same critics are somewhat mute about vegetarians and vegans – despite whole categories, namely meat or dairy – being omitted from the diet. It’s important to get some perspective on the scientific facts, and surely we owe it to the next generation to give them the best start in life?
So, we think it’s the right time to add gluten-free pregnancy and gluten-free weaning, to more established benefits that give babies a flying start, including vaginal delivery, breastfeeding for at least 6 months and circulating vitamin D in the optimal range (100-150 nmol/L [40-60 ng/ml]).
That’s why as part of September’s #ThrowbackThursday we’re sharing two of our previous articles on the problems that can be caused by gluten to give you the information needed to make a decision about whether or not you should go ‘gluten-free’.

What’s the big deal about gluten?
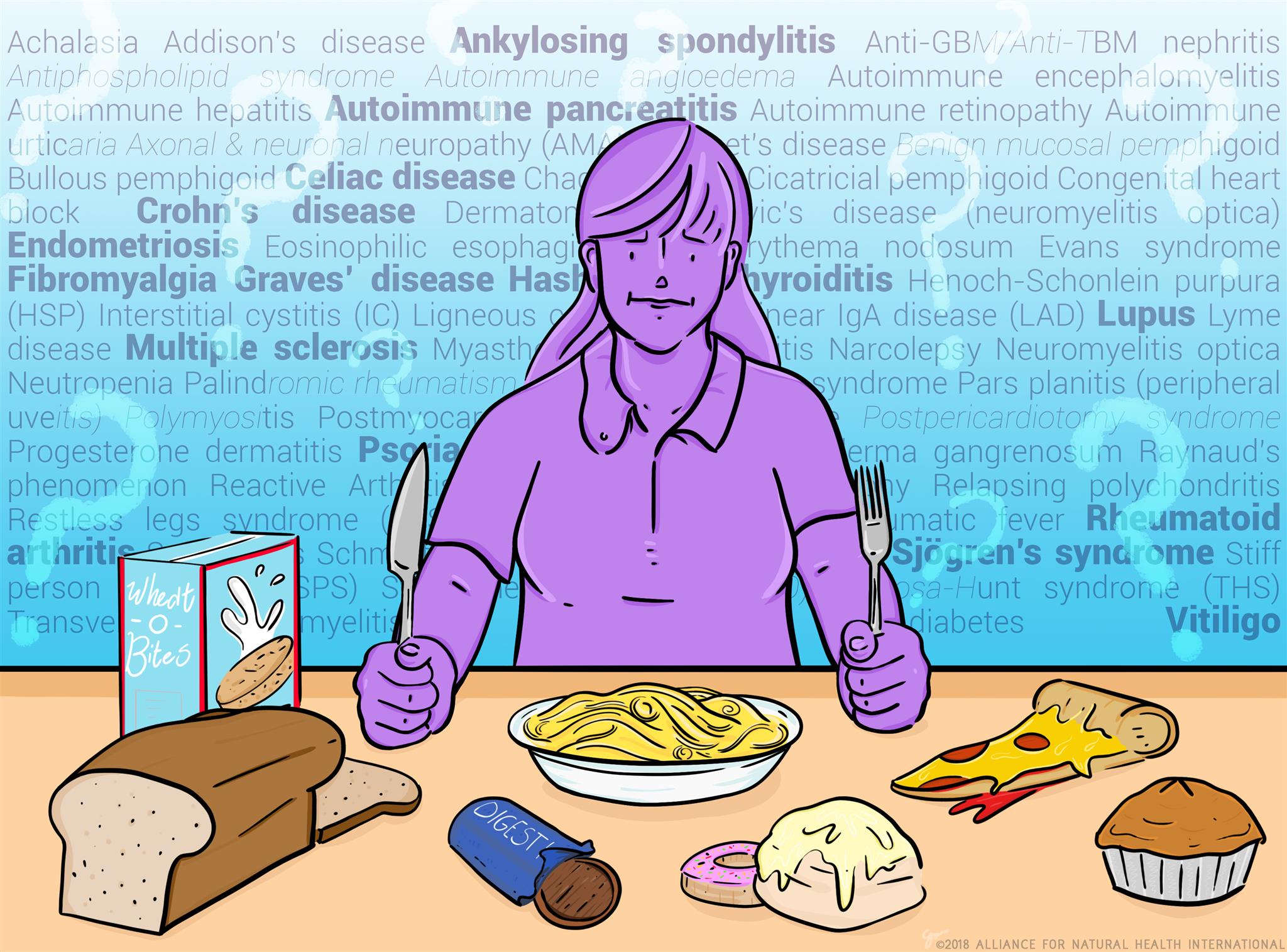
Up until recently, most people, whether members of the public or health professionals, thought a gluten free diet was only for the 1% or so of people diagnosed with coeliac disease. As research progresses and results from clinical practice emerge, we now know that gluten (a protein found in some grains) and associated proteins (gliadins and glutenins) can contribute to health issues in a much wider part of the population. The spectrum of gluten-related disorders broadly spans three categories: auto-immune, allergic and non-autoimmune/non-allergic conditions.
Gluten-related disorders
Widely acknowledged as the world’s leading expert on gluten-related disorders, Dr Alessio Fasano MD, along with his former team at the University of Maryland School of Medicine, Baltimore, proposed the following classification of the disorders (Figure 1), which may even be too simplistic.
Included among those affected by gluten are therefore not only coeliacs, but also people who suffer from wheat allergy (Ig-E and non-Ig-E-mediated) and those who have, what is now referred to, as Non-Coeliac Gluten Sensitivity (NCGS). First referred to in the 1980s, NCGS is the term used to describe individuals suffering a range of symptoms, not linked to auto-immune disease, that quickly improve after gluten is removed from the diet, and in which both coeliac disease and wheat allergy were properly ruled out. If gluten exposure is maintained, there is a risk that very serious conditions, such as autoimmune thyroiditis, may occur in around 1% of the NCGS population, itself difficult to estimate given the low rates of reporting and medical diagnosis.
Making matters even more complicated is the scale of under-reporting linked to gluten-mediated type 1 diabetes and cancer, both of which are triggered via autoimmune reactions (Figure 1). These conditions are frequently undiagnosed as being gluten-mediated and being forms of ‘silent coeliac disease’, they result from years, or decades, of chronic exposure to gluten.
Are you courting autoimmune disease with your daily staple?
In case you hadn’t noticed, as a society, we are now dying slowly (mostly uncomfortably and painfully) from chronic inflammatory and metabolic diseases, not fast from acute infections as our ancestors used to. Interestingly nothing much has changed in 40 years as far as genes and environmental triggers go, yet acute chronic disease rates continue to rise. Would it surprise you to know that we’re not born with the destiny to develop chronic inflammatory diseases (CIDs)? The stark fact is that our current health crisis is not down to genetic changes or pathogens (infections), it’s down to something we are doing to ourselves and the planet.
I’ve just had the extreme pleasure of sitting in 3-days of back to back presentations on all aspects of autoimmune disease (AID) at the Institute for Functional Medicine’s 2018 Annual International Conference. I know this might not seem like everyone’s idea of a good time, but we practitioners are a strange lot! The conference focused on the interplay of the gut, genes and the environment in an attempt to stitch together the ‘puzzle of autoimmunity’. Given that more than 100 autoimmune diseases have been identified, there was a lot of ground to cover. Yet, despite multiple diseases and multiple symptoms the causes and treatment approaches are often much the same.
Among the most important, known stimulators of autoimmune and chronic inflammatory diseases are gluten (the protein in wheat, barley, rye, spelt and triticale) and gut dysbiosis, aka unhappy gut bugs! Add obesity into the mix and you have the components in place for the perfect autoimmune storm.
This is a subject close to my heart as I developed Graves’ disease (an autoimmune disease) at the age of 17. Back then no one knew anything about the connection between gluten and autoimmune thyroid disease, so I underwent 2 years of extreme drug therapy. It didn’t work, and culminated in surgical removal of my entire thyroid gland (full thyroidectomy) at the age of 20. My passion for what I do in the natural health space was spawned the day I walked away from the surgeon’s office – young, vulnerable and still sick, but out of medical options. They washed their hands of me, job done. It took me 25 years to find what worked, but only 3 months to regain my health. No one has to suffer the same fate now we know how to prevent and treat gluten-related autoimmune disease.








Comments
your voice counts
04 October 2018 at 7:54 pm
Correlation does NOT equal "CAUSATION" people!
There must be numerous additional studies to confirm or eliminate Gluten as one of the HUNDREDS of food items that those in the study were exposed to!
One group with a curious correlation that the researchers were already trying to prove, means little to nothing in a properly run case study!
You are intentionally MISLEADING the public to enrich your own business!
SHAME on you!
06 October 2018 at 5:56 pm
Hi Steve, just FYI, we're not a business. ANH-Intl doesn't sell anything and isn't a commercial organisation. We're a non-profit, non-governmental organisation. Education and research are two key planks of our mission, campaigning and activism being the other two. As such, we have no vested interest in any products or in any research, but we are committed to supporting people to care for themselves and the planet using natural and sustainable approaches to healthcare.
Go well
Meleni
04 October 2018 at 8:21 pm
Glysophates are many fold more pro inflammatory than gluten-foods. I suspect more grains and higher concentrations of glysophates is the problem.
06 October 2018 at 6:05 pm
Hi Ralph, thanks for your comment. We do agree that glyphosate is definitely not something anyone should be ingesting, but avoiding glyphosate doesn't stop gluten creating gut permeability issues through it's triggering of zonlin (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3384703/). Gut permeability also drives chronic low grade inflammation, which is at the root of chronic disease and autoimmune disorders. So whether a single or combined effect, grains are some of the easiest foods to exclude from the diet and the difference to one's health is often dramatic.
Best wishes
Meleni
04 October 2018 at 11:01 pm
As a parenting author, speaker, columnist with a book in 18 languages, and a mother of three, I more than agree that grains and legumes as well as potatoes and sweet roots should not be part of a human diet, pregnant specially but not only. If it causes harm to the vulnerable fetus, then it causes the same damage to everyone, only takes long to show the harm. Even cancer and all autoimmune diseases can be reduced or totally prevented by avoiding foods made of substances that cannot be eaten without processing. Grain, beans, and many most roots are all not human food. They have to be "made" into food. They have toxins that ever after sprouting and processing still harm the human body.
However, raw eggs (specially the yoke) when organic from grass fed chickens or ducks, are an amazing health food for pregnant mothers and for all of us. Likewise small amounts of cheese from RAW organic grass-fed source are a fine source of much needed calcium for pregnant mothers as well as probiotics and other nutrients.
Eating nutrient dense foods that do not need to be altered from their natural state is best for pregnant women, children and all of us.
06 October 2018 at 6:34 pm
Thanks for your comments Naomi. As you know, this is can be a highly controversial area where people have very definite opinions. My personal view is that gluten-containing foods will in the future be regarded as one of the key environmental/health 'bottlenecks' of our time. Most people feel better when they exclude these foods, which include lectin-containing foods, which says a lot. As always, what we eat comes down to personal choice!
Best
Meleni
Your voice counts
We welcome your comments and are very interested in your point of view, but we ask that you keep them relevant to the article, that they be civil and without commercial links. All comments are moderated prior to being published. We reserve the right to edit or not publish comments that we consider abusive or offensive.
There is extra content here from a third party provider. You will be unable to see this content unless you agree to allow Content Cookies. Cookie Preferences