Content Sections
By Robert Verkerk PhD, founder, executive and scientific director, ANH-Intl
My inbox is currently awash with communications between different groups of scientists and clinicians who don’t see eye to eye on what constitutes the ideal human diet.
The two most polarised groups are vegans and carnivores. It’s akin to binary logic: advocates of 100% plant foods on one side, and those plumping for 100% animal derived foods on the other. But clearly, most people are neither. Somewhere in the middle is the continuum of what could be described as ‘compromisers’, those who see benefit from eating both plants and meat or other animal products, in varying amounts and ratios.
The ‘binarists’ might claim that compromising on plant and animal foods can’t be right, as that’s what the majority of people currently on planet Earth are doing – and most of those who do it are suffering dietary related health problems, from heart disease, obesity, type 2 diabetes through to neurodegenerative problems like premature dementia. Does that mean the ‘binarists’ have to be more right – or less wrong?
I don’t think so. And I will explain a little bit more about my thoughts on this in this short blog.
No one size fits all
The truth is that it’s impossible to come up with one dietary regime that suits every person on the planet. We’re all different genetically, some more than others – and we all live in unique environments. At the simplest level, some of us are able to handle certain foods better than others. Take dairy, for example. Only about 5% of people of Northern European descent are lactose intolerant, in contrast with around 90% of those of East Asian descent. The Inuits, who have traditionally lived off diets very high in protein and fatty acids, appear to have adapted genetically to these diets over generations. That means they’re not necessarily going to be applicable to those of Northern European descent.
We see evidence of similar adaptations in the Maasai and other cultures who have flourished at least to reproductive age on diets very rich in animal products, but who also rely heavily on plant medicine. By contrast, we need only look at the traditional Okinawans or Papua New Guinea tribesmen who appear to have done well on diets that deliver over 80% of their energy from plant foods and carbohydrates.

Purple, anthocyanin-rich sweet potatoes that represent the caloric mainstay of traditional Okinawan diets
From these and other data, we can deduce:
- Macronutrient ratios, namely the precise amounts or ratios of carbohydrate, fat or protein, may be less important to our survival, reproductive success or ability to live without chronic disease than dietary quality or other factors
- Amongst these other, food-related factors, is our access to food (less access = better for health), our feeding frequency (less frequency = better) and our ability to access an adequate diversity of plant foods, plant medicines and fibres that appear to be consistently associated with diverse gut microbial communities, longevity and resilience
- Additional non-diet related factors, particularly the nature and type of physical activity, its regularity, intensity and duration, appear to be important factors that interact, non-independently, with diet-related ones
- The effects of psychological, social and emotional factors have also been found to be strongly associated with heart disease, obesity and insulin resistance, among other risk factors, in different population groups
- Our exposure to new-to-nature industrial chemicals in our foods, air, water and personal care products undeniably pose significant health risks. However, we have particularly few data on real-life, combined exposures to multiple chemicals in relation to our individual detoxification capacity
- We also don’t have enough data on how all these factors interact with one another, and we have even less on how they relate to veganism or carnivory. Therefore we can’t draw hard conclusions about the long-term suitability of any one diet for most people on the planet. But we can postulate. And that’s one of the reasons the ‘compromisers’ often come out on top when you look at the balance of all the available evidence.
Trying to rationalise beliefs and experiences
While we know something about the many factors that affect our health and vitality, as well our risk of disease, we know a lot less about their relative importance for specific population groups. It’s no wonder then that any one of us can cherry pick data to suit our belief system or experience. Human nature being what it is, we can be much more persuaded when the information we choose to look at supports a consistent logic structure that both validates our belief system and supports our own experiences.
I find very few, if any, relevant data from human trials, such as prospective cohort studies, or from epidemiological studies, that support the long-term safety and benefits of full-blown carnivorous diets in Western humans living in industrialised societies. However, I hear, loud and clear, the revelations among clinicians and patients who report rapid recovery from auto-immune conditions or successful weight loss when all plant foods are removed from the diet. Take the plant ‘noise’ out of a dysregulated immune and endocrine system, and that can be the start of a healing journey. But it may not necessarily mean it’s the end of it.
Critically, these short-term benefits should not be confused with long-term safety, or the denial of extensive evidence of the long-term health benefits and resilience associated with consumption of diverse, plant-based diets, which may or may not include significant amounts of animal-derived foods.
Complicating matters further, we have to also recognise the likely impact of the last century or so of plant breeding and changes in cultivation method. Let me be controversial: these changes may be even more impactful to health than the introduction of genetically engineered crops. They have resulted in huge changes in phytochemical profile and relative amounts of digestible and indigestible (fibre) carbohydrate, as compared with traditional plant-based diets that originate from traditional cultivation and food preparation methods.
That’s why I find it useful to think of knowledge, most of which is extremely limited given we’re still in our infancy in understanding human nutrition within an ecological and epigenetic context, as distinct from our belief systems (see Figure below).
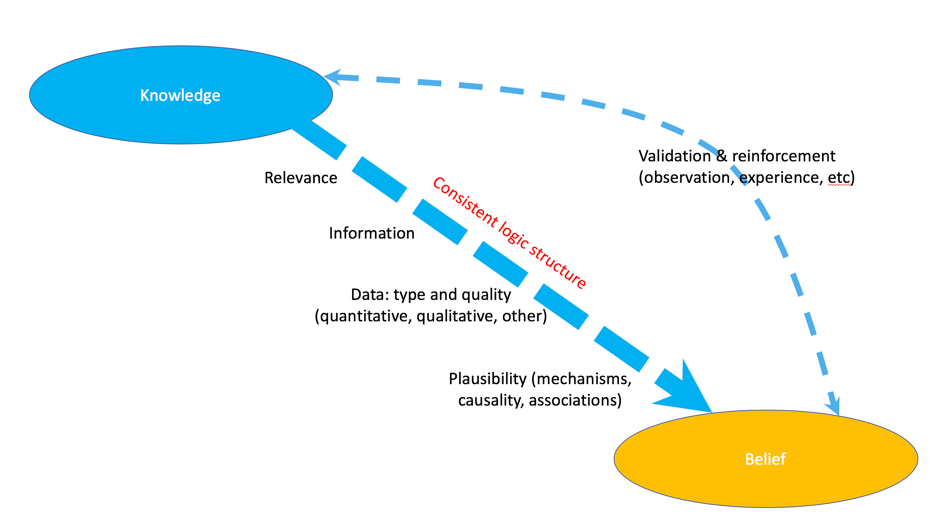
Figure. From my presentation entitled “Shifting paradigms in research outcomes” given at the Royal Society of Medicine, 14 July 2018, adapted from information in Friedkin NE et al. Network science on belief system dynamics under logic constraints. Science. 2016; 354(6310): 321-326.
Where to in the mists of confused or unclear science?
Should we bury our heads in the sand and leave scientists and governments to argue it out? Absolutely not! For those of us interested in using diet to optimise our health in the short- as well as the long-term, we must do what appears to work best for each one of us. That’s what our health sustainability ‘blueprint’ is all about – a system that helps us to evaluate what works for each one of us, genetically different individuals, living in unique and often highly varied, dynamic environments.
In the meantime, if you’re going to compromise and look at what many people appear to do well on, getting the best of both worlds (fatty acids, protein quality, micronutrients, polyphenols, fibre, etc) makes rational sense given all the available data and information. That includes taking into account the thorny, complex and multi-faceted issues of human and environmental sustainability.
And it’s from this non-binary place that the scientific, clinical and experiential evidence that underpins our Food4Health guidelines originates. But remember: diets are about choice, rather than obligation. In the light of such limited and contradictory information about human diets, the only views on diet I tend to dismiss are ones that are rigid and universally applicable.








Comments
your voice counts
05 December 2018 at 10:13 pm
While all that you write is important, the most critical aspects of diet narrative 'wars' that then support regulatory structures of sickness, are around the 'overcontrol' corporate management systems that can extend from logical compensations to logical extension of negative impulse of domination, and subjection.
So at one end are profit models and margins of food as economic inputs and outputs, which if not required to serve life will simply organise life to serve it.
And at the other are the manipulative 'identity' politicking of guilting or inducing fear as the basis for then imposing heavier controls backed by the emotional investment as a social narrative.
I hold the demonisation of carbon dioxide to be no more scientific than Ancel Keys studies on fats - and to serve a similar purpose of diversion and catchment. Diversion from sugar awareness into the consumption industrial fats or oxidising and trans fats along with the 'low fat' diet and cholesterol fears that have NOT served health and well being but undermine us. The CO2 issue has in effect captured and targeted environmental awareness into a singular issue that has been set by political will as an imperative and overriding threat that displaces almost all others and there are very many toxic and environmentally degrading practices that are thus diversioned from - with a captive identity of saving the Planet or being a 'denialist'. Veganism as a top down corporate intent is different from being a freedom of personal choice and links in with more PR disguised as science, using 'carbon guilt' to ally with 'meat guilt' for a manipulative agenda in which offences against vegan sensitivities can be empowered along with offences against the Planet to merit regulatory limitation or taxing, as well as defining new crimes as is being orchestrated with regard to other freedoms in a once tolerant society, so as to become intolerant under a sense of self righteousness.
While I don't eat highly processed foods, it is apparent that the 'vegan' masking is being rolled in as a 'health' and 'planet saving' alternative to low fat high sugar 'foods', (or indeed low sugar high aspartame).
The freedom to choose to eat or not eat meat is not in question here. The denial of other's freedom under false pretences is. As for the anti LCHF and associated diets - this is simply a war on revealed truth. Not that such a diet should be mandated or that individual needs are in fact individual, but that drugging and stupefying the population with refined carbs/sugars of low nutritional value is a policy and not a mistake.
The consent to being managed by systems that are blind or malign, is a form of slow suicide. We don't ask for the right to withdraw consent, but exercise it. Insofar as there is a willingness to serve the whole, let the systems and logistics mind attend and support. But not to hold captive and abuse.
06 December 2018 at 12:15 pm
Thanks for a very thought provoking article. Could I suggest that one important factor is to take care to adopt methods to maximise ones ability to integrate diverse knowledge into a coherent whole. Science involves analysis and synthesis and not enough attention is given to enhancing the latter.
What methods enhance ability to integrate knowledge? A subject for several blogs I think!
Your voice counts
We welcome your comments and are very interested in your point of view, but we ask that you keep them relevant to the article, that they be civil and without commercial links. All comments are moderated prior to being published. We reserve the right to edit or not publish comments that we consider abusive or offensive.
There is extra content here from a third party provider. You will be unable to see this content unless you agree to allow Content Cookies. Cookie Preferences