Content Sections
Download PDF - Full 140+ page ANH-Intl Blueprint for health system sustainability
Download Executive Summary only
Download Blueprint Health System Sustainability presentation deck - 21 slides distilling the essence of re-imagining health and care through the lens of sustainability
If you want to have a deeper understanding of what our sustainable health project is all about, why it might matter to you, as a citizen, a practitioner, or a company involved with natural health, try and find yourself a spare 47 minutes to listen to this podcast as Rob Verkerk PhD speaks to Ben Brown ND.
By Jerome Burne and Rob Verkerk PhD
The claims of the new ‘sustainable health’ approach – as outlined in our December 2018-released blueprint – may seem wildly optimistic at first sight. Could it really cut the risk of such major killers as diabetes, cancer, heart disease and Alzheimer’s that are now breaking the back of the NHS and other health systems? Surely not, without some kind of major medical breakthrough, and only with little more than diet, exercise, a few lifestyle changes and recourse to a wider network of health practitioners? Haven’t doctors been telling patients for decades that eating less and moving more is the way to stay healthy while the number of diabetic and obese patients soared? What’s so different about this remedy – ANH's sustainable health blueprint?
Needing to get radical
The answer is that the approach outlined in our blueprint, that includes elements of functional, integrated and lifestyle medicine, while looking at each individual as a unique entity functioning in a complex and dynamic ‘ecosystem’, is radically different and far more sophisticated. Three big differences are that:
-
It’s much less concerned with treating or managing diseases and much more concerned with creating or regenerating health
-
It offers a common language that can be used by citizens and all types of health (and fitness) practitioner so that the individual understands much more about what's going on in the body and so becomes empowered. The common language means it's easier to see which specific areas of health should be prioritised, as well as identifying particular 'tools' that can be used to monitor each major area. Amongst these are comprehensive biomedical and genetic tests. Finally, it also allows the individual to select particular modalities of health professional most suited to offering relevant guidance
-
The approach prioritises non-pharmaceutical approaches that focus on balancing 12 distinct domains of human health. It shows how we can move from the ‘silos’ of the medical mainstream and the sometimes disconnected modalities of integrative and alternative medicine, towards a participatory and collaborative approach that puts the individual right at the centre.
Doctors or practitioners who adopt a sustainable health approach to their practices pay attention to the state of the major systems that determine how well or disordered our bodies are. The blueprint identifies 12 areas or domains that make up our ‘ecological terrain’, the ground of our being, and everyone’s is different, subtly or significantly. They include our genetic background, hormones and inter-connected nervous system, our blood glucose regulating capacity, the state of the vast microorganism colonies in our guts (microbiome) and, amongst other things, our ability to relax and handle stress. Today, most GPs who run annual check-ups focus mainly on markers for just one system: the cardiovascular system.
Fundamental to the effectiveness of the holistic approach detailed in the blueprint is the involvement of the individual. It’s important to not think of us, the recipients of ‘health care’ as patients, given that ideally health care is something we engage with on a daily basis even when we’re in apparently good health.
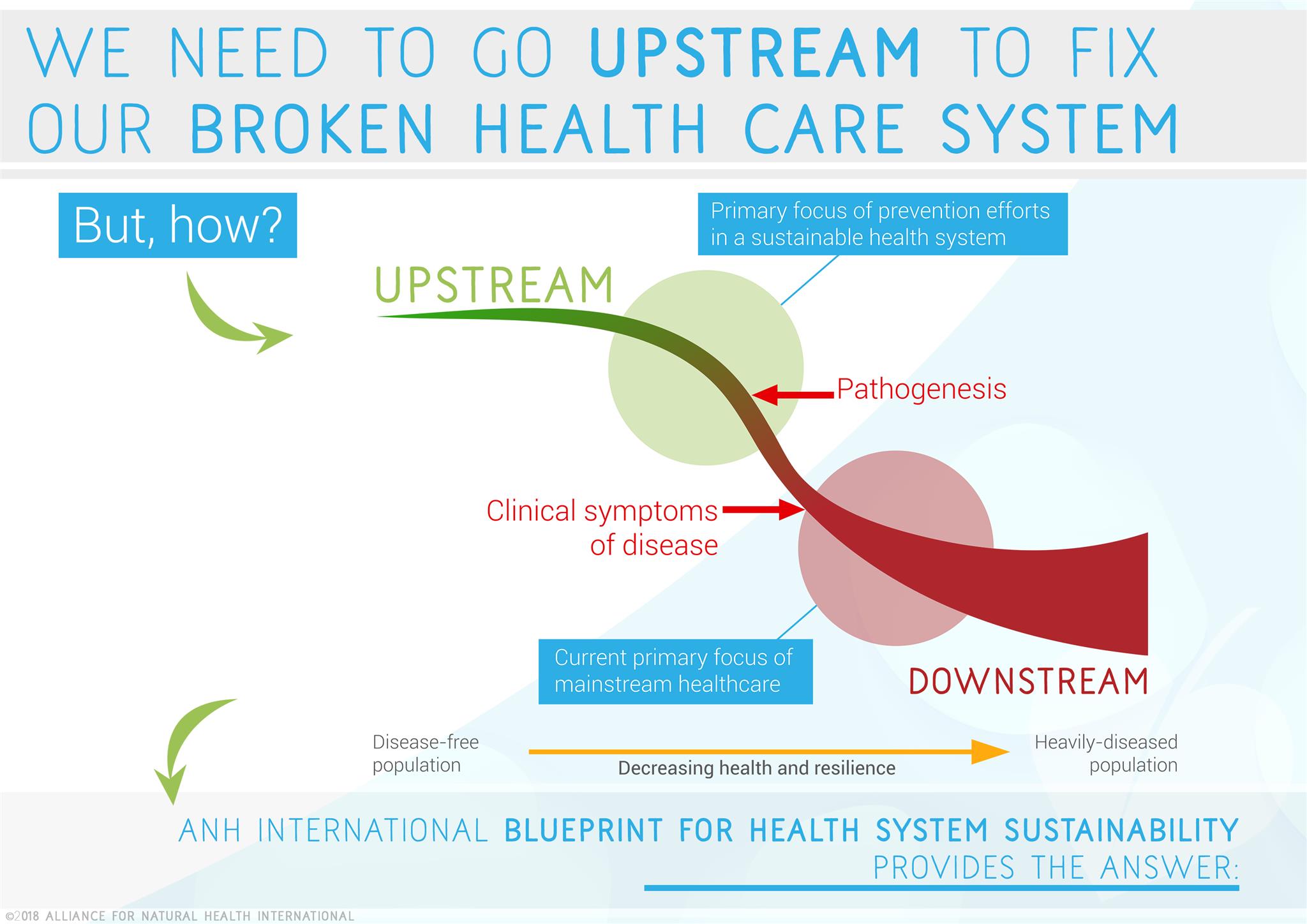
Looking upstream
The blueprint proposes that we move towards an ‘upstream’ model of health care and self care, one that aims to keep all the major systems of the terrain in balance to optimise health, as early as possible in an individual’s life.
Waiting for a ‘car crash’ – the clinical manifestation of any number of debilitating, downstream diseases – and then trying to pick up the pieces and restore a body to some semblance of health is not only an often ineffective way of going about doing health care. It is also a very expensive way of doing it. Many diseases, especially chronic ones like type 2 diabetes, obesity, coronary heart disease, Alzheimer’s and many forms of cancer or autoimmune disease, are related to inappropriate eating and lifestyle patterns. Evidence shows us these conditions can be difficult or impossible to fully reverse if they are addressed late in the disease cycle. The outcome can be very different, however, if you intervene early enough.
Re-educating doctors
A major challenge is that most GPs just don’t have the training or experience to help people with these kind of changes in their lives. As a result, organisations like Clinical Education, a formal endorser of the blueprint, are attempting to fill the knowledge gap among British GPs. Dr Ayan Panja, a GP and a presenter on BBC News, together with Dr Rangan Chatterjee, who fronts BBC One’s Doctor in the House, are now facilitating courses on Prescribing Lifestyle Medicine which have been accredited by the Royal College of General Practitioners.
“New research clearly shows that the sort of food you eat, the balance of bacteria in your guts, your sleep patterns and the way you handle stress can all affect your wellbeing, right down to the level of cells and genes,” says Dr Panja. “Right now, GPs rarely have much specific to say about any of them.”
The blueprint’s bottom-up, sustainable approach to health and care could be rapidly put to test in real world settings. Positive outcomes could, in turn, catalyse rapid roll-out in communities in order to tackle a wide swathe of preventable causes of the lifestyle epidemics that now present the greatest burdens on health care systems the world over. The blueprint, in its Recommendations, shows how this can be done.
Why ‘eat less, move more’ is doomed to failure
Current advice to eat less and move more simply doesn’t work. That’s largely because it's based on false scientific and medical premises, especially insufficient understanding of the underlying disturbances to normal function as seen in the terrain. The regular consumption of foods and snacks based on refined carbohydrates in many people’s diets results in repeated episodes of raised blood glucose. The pancreas responds by elevating blood insulin and excess glucose is shunted into cells and stored as fat. To boot, the consistently raised insulin levels tells the body to hold on to its fat stores, putting a block on the body's ability to burn fats for energy, let alone produce ketones from the liver (the energy carrier we use when we're fasting).
But that's not all. Then the fat stores, especially the visceral fat around the waist, send out messenger molecules (kinase signaling) which can reduce the normal feeling of fullness after a meal and ramp up the production of a hormone (ghrelin) that make you feel hungry even when you've got ample energy stores on board. Levels of another hormone, adiponectin, that helps the body burn fat and reduces insulin resistance, are also suppressed. Eating significantly less and having the capacity to burn fat in this metabolically dysregulated state is almost impossible and explains why the latest drive by Public Health England to tackle obesity by recommending just eating fewer calories at every meal is doomed to failure.
If attempts are not made to reverse this pattern of hormonal imbalance, it is likely to trigger further damaging states. These include persistent, systemic low-grade inflammation, a rise in the release of damaging oxidants from the energy-producing units (mitochondria) found in nearly every cell and a shift in the balance of types of bacteria in the gut. These kinds of changes are all linked with other big chronic disorders such as some forms of cancer and Alzheimer’s.
Where’s the evidence?
A common response to the ambitious claims of 'integrative medicine' as well as the different modalities of complementary and alternative medicine (CAM) is to demand evidence. This seems reasonable, but it raises the question of what is the best way to gather that evidence? The gold standard for drugs is the Randomised Controlled Trial (RCT) which compares two matched groups with a given condition, one getting the drug, the other not. The reputation of RCTs, for better or worse, has been tarnished by a long history of commercially driven manipulation of results. But even in mainstream medicine, the number of treatments supported with good evidence is actually quite small – only around 11% – according to the recently disbanded clinical evidence unit of the British Medical Journal.
The relevance of RCTs to evaluating the complex combination of treatments that lifestyle and integrative medicine uses is debateable. Not only are RCTs hugely expensive, the primary funders of medical research over the last half century or so – the drug companies – are not interested in funding trials for non-drug interventions such as dietary or lifestyle changes, let alone CAM.
Also, many of the approaches designed to change the function of a given domain of the terrain vary from individual to individual and include things we all do every day such as eat and sleep. That makes comparisons designed to yield the precise influence of a single therapy difficult or impossible.
Real World Experience vs Randomised Controlled Trials
An alternative approach is to record the changes in a person’s health status (perceived or actual) or the function or status of their biological terrain, according to all the influences to which they’re exposed in the real world. Some of these people, even if they are heavily reliant on non-drug approaches, may be taking pharmaceuticals as well. This kind of real world scenario is fully taken on board in the blueprint.
At ANH-Intl, we are collaborating with other partners, including the insurance company Balens, the Netherlands-based contract research organisation TNO and others in the Hawthorn Health Collaboration to create an app, called GoHawthorn. The app will allow individuals to evaluate their health and compare their own health trajectories with others using a big data approach.
Available tools and interventions, however, aren’t limited to diet and lifestyle changes that only help to improve the metabolism or physiology. They also include a diverse range of modalities that help influence emotional and psychological functions. Negative emotional states resulting from trauma, stress or social conditions such as loneliness, or a lack of purpose or meaning in life, can have big impacts on an individual’s health and resilience. One way is by raising the stress hormone cortisol which, among other effects, can reduce the levels of various brain chemicals such as serotonin and dopamine, a lowering of which is linked with depression.
Take homes
Three of the biggest contributors to the burden on the UK’s NHS are obesity, type 2 diabetes and the impacts of chronic, psychosocial stress. These conditions have a range of knock-on, downstream effects that are so serious, they threaten to render the healthcare system, as we know it, unserviceable for future generations.
The blueprint is about providing an approach that is future-fit. It focuses not on the problem, but the solution. It isn’t exclusive to one system of medicine, it is inclusive of all systems.
We know that change won’t happen until enough people with a common goal get on board with the same vision. Using the lenses of sustainability and ecology, we’ve sought, through extensive research, as well as through wide collaboration and consultation, to find an approach that has universal appeal.
If you care about the kind of health care system we might leave to the next generation, we urge you to digest our blueprint.
If you like what you’ve read, please share it among those who share our vision. Think carefully about which of your friends, family, health professionals and elected representatives might come on board with our vision for change.
Together – the much-needed revolution in the way we go about managing our health – can begin. Not a minute too early.
Download PDF - Full 140+ page ANH-Intl Blueprint for health system sustainability













