Content Sections
- ● An example to highlight the differing perspectives: abdominal pain
- ● The dietetic approach
- ● The nutritional therapy approach
- ● ‘Fill up on sugary desserts, sweetie’, says the Royal Marsden to its cancer patients
- ● What is dietetics?
- ● ‘Evidence based’: what does it mean?
- ● Dietetics and evidence-based medicine
- ● Nutritional therapy and functional medicine
- ● Jeffrey Bland PhD summarises how functional medicine provides an appropriate model for 21st Century medicine
- ● The evidence for functional medicine
- ● Conclusion
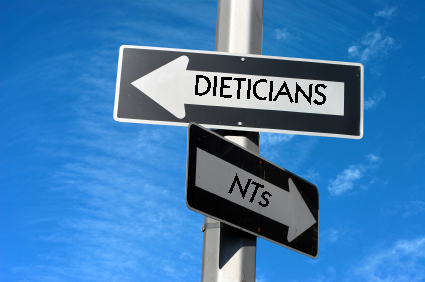
As we pointed out in our article on the recent Which? investigation of nutritional therapists (NTs) in the UK, NTs and dieticians are very different animals. Although the Which? article contained many inaccuracies and biases, what shone out clearly from the investigation was that anyone visiting a dietician with a particular condition would likely receive very different advice if they went to see an NT. But why is this? This article attempts to shed some light on the different approaches of NTs and dieticians.
An example to highlight the differing perspectives: abdominal pain
Let’s look at something commonplace: abdominal pain. In fact, abdominal pain is given as the number one reason members of the UK public call NHS Direct for advice. Symptoms of gastrointestinal (GI) distress are so usual these days that many people accept their wind, bloating, cramps, diarrhoea or constipation as normal. But they aren’t normal for a healthily functioning digestive tract. Anyone suffering from abdominal pain that seeks help from a practitioner may receive hugely differing advice, depending on whether they see a dietician or an NT. Of course, advice from an NT is also likely to differ significantly between patients, as the advice tends to be individualized, and no two people have the same genetic, social or environmental backgrounds.
The dietetic approach
Dieticians, as registered healthcare professionals allied to conventional medicine, are entitled to treat named medical conditions and may well acknowledge such a group of GI symptoms as irritable bowel syndrome (IBS). Guidelines from the British Dietetic Association (BDA), in association with the National Health Service (NHS), give recommendations such as eating regular meals, not skipping meals or eating late at night, eating slowly and chewing food thoroughly and taking regular exercise and relaxation. They also recommend certain dietary changes based on the symptoms experienced — such as reducing fibre and resistant starches (e.g. wholegrains, nuts, seeds, potatoes) for those suffering with wind and bloating, and increasing fibre and wholegrains for those experiencing constipation. Fluid intake of 8 cups per day is recommended, and this includes water, non-caffeinated fluids, herbal teas and sugar-free squash (cordial). Fizzy drinks are limited but not excluded, as are caffeinated drinks and alcohol, for those with diarrhoea, while there are no such limits for people with constipation.
The BDA IBS guidelines do mention keeping a symptom diary; however, they also make it extremely clear that, while symptoms are likely to be related to food consumption, “True food allergies are rare and are unlikely to cause IBS. However, IBS symptoms could be caused by food intolerance. There is no convincing evidence to support any of the commercially available food intolerance tests. If you feel your symptoms are due to food intolerance, ask your doctor to refer you to a registered dietitian”. However, dieticians tend to recognise food allergies (e.g. nuts, gluten) more than they do food intolerances, and advise against avoiding major food groups, such as wheat and dairy, to prevent deficiency of vital nutrients.
The nutritional therapy approach
NTs, on the other hand, recognise that chronic, low-grade, systemic inflammation sits at the heart of all chronic disease. Certain foods and food groups can cause or exacerbate inflammation in sensitive individuals, leading to food sensitivity and food intolerances. NTs do not diagnose or treat medical conditions, such as IBS, but instead support the underlying health of the body to help it function more optimally. This support takes the form of both nutritional and lifestyle advice, and can also involve the judicious use of food (dietary) supplements and, if deemed necessary, functional testing. The result is an individually tailored, patient-centred programme providing a roadmap to an improved state of health and vitality.
In the case of GI disturbance, NTs would attempt to uncover the triggers and identify the possible sources of distress. Years of experience with Western diets has shown clearly that the most common foods to which sensitive individuals can react are cereals (especially wheat) and dairy, but a compromised GI tract can also be reactive to other foods until optimal function is restored. During the consultation, an NT will spend time with the patient looking in-depth at the antecedents, mediators and triggers for the patient’s current state of health. Importantly, the consultation focuses on the patient’s whole body and health history since birth, rather than just looking at the presenting disease symptoms.
Exclusion diets are the simplest and cheapest way of establishing if a food or food group is causing some type of reaction. Conventional testing for food allergies may not reveal all intolerances and sensitivities, but removing a suspect food for a short period of time, e.g. 4 weeks, and then re-introducing it again usually gives a very clear response. Dietary exclusion programmes take care to replace and augment any essential nutrients lost as a result of the exclusion by increasing intake of other food groups.
Any nutrition plan from an NT is typically based on whole, unprocessed foods. NTs also take care to recommend a diverse range of complex phytochemicals and enzymes – hence the catchphrase: “eating a rainbow every day” – while strictly avoiding synthetic food additives, colourings and preservatives, as well as artificial sweeteners. Finally, NTs treat water as a separate group from ‘drinks’, with a recommended daily intake of around 1.5 L for an adult.
‘Fill up on sugary desserts, sweetie’, says the Royal Marsden to its cancer patients
The main plank of dietetic advice to cancer patients at the UK’s prestigious Royal Marsden hospital illustrates perfectly that advice from NTs and dieticians is worlds apart. Here, vulnerable cancer patients are encouraged to eat as many calories as they can – regardless of where those calories come from. Highly processed, sugary foods, including Angel Delight, Instant Whip, Aeros, Rolos and Dairy Milk, are all recommended as high-calorie food sources, alongside an extensive list of other desserts, curries, pasta, pizza and so on. Patients are recommended to swap “low energy foods such as vegetables and fruit” with high-energy foods, such as puddings, if they find they have a reduced appetite. This approach runs completely counter to that of the NT, who would never recommend highly processed and sugary foods to anyone as a useful part of their diet, whether healthy or sick.
What is dietetics?
It’s obvious that the differences in theory and approach between dieticians and NTs are not trivial. But is it really – as dieticians would have us believe – because NTs are basically making it all up: “[NTs] do not use the evidence in a robust fashion and advice is most often based on personal opinion or belief”? To answer this question, we need to understand what dietetics is and how it views its place in the medical landscape.
The BDA describes dietetics as, “The interpretation and communication of the science of nutrition to enable people to make informed and practical choices about food and lifestyle, in both health and disease.”
Since dietetics is the accepted nutritional counterpart to conventional medicine, it must also be accepted that dietetics does not try to replace drugs, radiation or surgery, the three main pillars of conventional medicine. Instead, it acts as an add-on, generally ensuring that a patient is adequately nourished given the very limited framework of evidence that dieticians are prepared to accept. The contempt that most dieticians have for NTs is based on an incorrect belief that nutritional therapy is not evidence based.
‘Evidence based’: what does it mean?
While multiple definitions of ‘evidence-based medicine’ (EBM) exist, the original definition by Prof David Sackett and colleagues from the Centre of Evidence-Based Medicine at the University of Toronto, Canada, stressed that EMB practice should integrate three things:
- Individual clinical expertise
- The best available external clinical evidence from systematic research
- Patients’ values and expectations
Unfortunately, EBM, in the minds of the majority of primary healthcare providers, largely relies on just a part of only one of these three legs. Thus, if a double-blind, placebo-controlled, randomised, controlled trial (DB/PC RCT) hasn’t shown a statistically significant effect, the intervention remains unproven and therefore invalid. Worse, if a DB/PC RCT has not been conducted, the intervention also remains unproven and invalid – even if research has not been performed because commercial interests have not seen any prospects for making money on the back of the findings. From this ultra-narrow EBM perspective, an intervention with plenty of biochemical, molecular and genetic evidence in its favour, plus decades of positive clinical experience, will tend to be viewed as without merit. And of course, patient values and expectations rarely get much of a look-in.
Dietetics and evidence-based medicine
Dietician advice is based on similar criteria to that now used in the ultra-narrow variant of EBM. Given the hierarchy of evidence used, this means a dietician’s first port of call for evidence will typically be a source such as the Cochrane Collaboration or Bandolier. These databases provide exactly what the RCT-evidence-only-brigade wants: clean, simple conclusions for given interventions based only on RCTs.
Systematic reviews and meta-analyses (studies of studies) are often accepted on blind faith, with no attempt to understand such things as study design, assumptions inherent in the design or the shortfalls of each study reviewed. Above all, no consideration is given to each review’s applicability to an individual with his or her unique genetic constitution and life history. RCTs invariably explore the effect of one or a very limited range of variables. With such a narrow view of evidence, most mainstream dieticians appear to assume that, if an RCT has not been conducted for a given food/nutrient interaction, the effect is either unimportant or does not exist. That’s why dieticians continue to advocate whole grain cereals, without necessarily taking into account the high prevalence of gluten sensitivity in Western populations exposed to wheat as a staple.
Dietetic science draws very little from the rapidly evolving sciences of molecular genetics, evolutionary biology and systems biology that provide the scientific framework for functional medicine (FM), the scientific and clinical practice discipline that underpins nutritional therapy. It is highly unlikely that a robust evidence base exists for the use of Angel Delight, Instant Whip, Aeros, Rolos, Dairy Milk and other such foods, and yet their use doesn’t appear to be questioned. Nutritional advice is never straightforward, and it is worth bearing in mind the considerable literature on the benefits of caloric restriction in managing certain cancers; such an approach would never advise the consumption of sugary desserts in place of cancer-protective vegetables and fruits.
Nutritional therapy and functional medicine
Anyone choosing to consult one of the most authoritative textbooks on functional medicine, Textbook on Functional Medicine (2010 edition), Institute of Functional Medicine, 906 pp., would have difficulty making the case that FM is not evidence based. And in case anyone doubts the linkage between nutritional therapy and FM, this textbook is the primary reference to clinical practice in nutritional therapy given by the British Association for Applied Nutrition and Nutritional Therapy (BANT) on its website.
The roots of FM go back around 30 years, in the USA, when a group of passionate medical doctors, researchers and naturopathic physicians decided that a new model of healthcare was needed. Their new model would particularly deal with the complex, chronic diseases that represent the biggest healthcare burdens on Western societies. While FM sits on the cutting edge of healthcare, there are particular elements of FM that are at the opposite end of the spectrum to conventional medicine. Conventional medicine, for example, is disease-diagnosis and treatment centred; while FM helps manage an individual’s environment in such a way that his or her unique response is optimised, taking into account genetic predisposition and make-up.
The contrast between the FM and conventional medical models is aptly summarised in a short interview with Jeffrey Bland PhD, one of the originators of the FM concept, given at the 2011 Integrative Healthcare Symposium (March 4–6, 2011, New York).
Jeffrey Bland PhD summarises how functional medicine provides an appropriate model for 21st Century medicine
Those interested in further detail can view more short videos by other leading figures in the functional medicine area, also recorded at the 2011 Integrative Healthcare Symposium.
The evidence for functional medicine
So, what is the evidence base of FM? While there is an increasing body of clinical trials supporting particular FM approaches, FM’s main thrust is toward understanding an individual’s uniqueness – a product of a lifetime’s interaction between that individual and his or her environment. Therefore, FM places great emphasis on identifying imbalances in metabolic systems, as opposed to diagnosing disease, an area that has been claimed exclusively for orthodox physicians via regulatory systems in most parts of the Western world.
Conclusion
We hope this helps to clarify that conventional medics, dieticians and other detractors are ill-informed when they dismiss nutritional therapy as, “Not us[ing] the evidence in a robust fashion and advice is most often based on personal opinion or belief”. Dietetics and nutritional therapy are two different theories and worldviews that attempt to bring some sense to the immensely complex area of human nutrition. We shall see in time which approach turns out to be the more valid, effective and ‘evidence-based’, and also which provides the most appropriate answer to the complex epigenetics facing modern humans. In the meantime, we encourage prospective patients to follow their instincts and choose the nutritional path that feels the most appropriate to their circumstances. And to remember that the rapport between the patient and the practitioner is a key part of the process, so take time to choose the right practitioner too.







Comments
your voice counts
27 January 2012 at 7:16 pm
Thanks for highlighting the shocking dietary advice given by the Royal Marsden. As someone who was treated there for cancer myself over ten years ago I did complain about this, as have others, but seemingly to no avail.
Luckily I ignored their advice and got better from Stage IV melanoma with a strict naturopath-prescribed diet.
This is a great article. Thanks.
31 January 2012 at 5:32 pm
Hi. I couldn't agree more with your comments and the differences between these professions. It is such a shame. I am a clinical dietitian (studied in Australia) and do not believe in sweets and puddings as nourishing foods for cancer petients! I left university feeling very disillusioned with what I spent 4 years studying... I have since studied Functional Medicine and currently continue my education with IFM. I think however I am a rare breed, usually dietitians are dietitians! I would be interested if there are any other people in this position?
13 February 2012 at 3:11 pm
Thank you for clarifying the differences so eloquently.
13 February 2012 at 3:12 pm
Thank you for clarifying the differences so eloquently.
30 November 2014 at 10:00 pm
I am very keen to pursue a career in Nutritional Therapy, could you recommend a certified course in London?
21 January 2016 at 8:19 am
The first link in the "Conclusion" paragraph is now disfunctional. I suppose they realised their error and changed the dismissive approach. Or re-phrased it?
Great article, like many others you produce.
Oliver Dowding
21 January 2016 at 12:03 pm
Thank you for drawing our attention to the disfunctional link Oliver. It looks as though they have removed their article as I can't seem to find it elsewhere on the website.
Many thanks.
24 July 2024 at 2:26 pm
I wholeheartedly disagree with this post and believe it is massively underestimating the care, attention and evidence-base that Dietitians bring to the assessment and treatment of patients, not to mention the four years of training, clinical placement, extensive training in statistical analysis and the critical analysis of research and studies that informs how we change our care as new empirical data comes out.
It's a shame that the comments from the Royal Marsden are (likely) taken out of context. Often times, patients with certain aggressive cancers - such as pancreatic, throat or stomach cancers - will struggle an incredible amount to eat, digest, and assimilate foods effectively. Our palettes change from harsh oncological interventions, and thus our food preferences change - we find the foods we once tolerated taste 'metallic' or lose their intense flavour, making us crave different, perhaps more hyper-palatable foods.
This poor intake often leads to conditions such as sarcopenia and poor immune function, which is associated with poor outcomes, and often resulting in patients requiring breaks or cessation of chemo or radio treatments that could be life saving/preserving. It may be that the message is more 'eat what you can, eat what you like, and try to eat well' rather than 'eat sugary foods and ignore all else', because calories are hugely important to the prognosis and quality of life of someone with cancer, and those with terminal or end-of-life disease states deserve to have an end of life that is dignified, and have their wishes and preferences respected, without someone suggesting an alkaline, low-inflammation juice-based diet that feels punishing and cruel. Once a patient recovers from treatment, the recommendation would always be to eat healthy, balanced foods. We care deeply about our patient's health and ensuring they have all the information to make an informed decision, but within that discussion, is the acknowledgment of someone's mental and emotional wellbeing. A slice of cake now and again has never and will never harm anyone.
Unfortunately, like many things in life, nutrition is not sexy. The evidence over the past 50 years has been fairly unwavering, even as our ability to do better research has improved- but that doesn't stop our society and industries from wanting to create new fads to sell us more supplements, diet plans, 'medical treatments', IV drips, and wellness regimens.There are many debates here and there about saturated fats causing heart disease - and then we find out about cardio-protective microlipids - and then we learn about the nuances between processed and non-processed sources of sat fats and how that can affect our health differently, and yet the evidence-based recommendations stay relatively unchanged. Carbs are bad, then good, then bad, then good, protein is fetishised beyond belief, with 8 year olds asking for scoops of whey powder in their smoothies for breakfast, and 'inflammation' might as well have it's own PR team. Old, fad diets are simply being wrapped up in new packaging under the guise of diet culture and fear of disease/aging.
It takes a scientific, non-biased, critical and evidence-based eye to decipher what would really benefit the patient vs what is harmful on a physical and psychological level. Being associated with a body such as the British Dietetic Association AND HCPC ensures that although our advice might be simple, and often times boring, it is safe and effective.
Your voice counts
We welcome your comments and are very interested in your point of view, but we ask that you keep them relevant to the article, that they be civil and without commercial links. All comments are moderated prior to being published. We reserve the right to edit or not publish comments that we consider abusive or offensive.
There is extra content here from a third party provider. You will be unable to see this content unless you agree to allow Content Cookies. Cookie Preferences