Content Sections
By Rob Verkerk PhD, ANH founder, executive and scientific director
Listen to the article
Read the article
The UK, like many other countries in the Western world, is grappling with a surge in long-term sickness that threatens to overwhelm the National Health Service (NHS) and puts immense strain on the economy. That’s before you look at the cost on the quality of life of hundreds of thousands, those affected both directly and indirectly. While there’s no doubt that the COVID-19 pandemic exacerbated this trend, the roots of the crisis run deeper, revealing a complex interplay of factors contributing to a nation that’s becoming progressively more sick, less capable, and less resilient. Rule Britannia? Hardly.
A Stark Reality in Numbers
Official statistics paint a grim picture (Fig. 1). The Office for National Statistics (ONS) reports that the number of Brits economically inactive due to long-term sickness has skyrocketed by half a million since 2019. This rise is unprecedented and represents a significant challenge for policymakers and healthcare providers alike. As of July 2023, over 2.5 million people of working age were out of the labour force due to long-term illness.
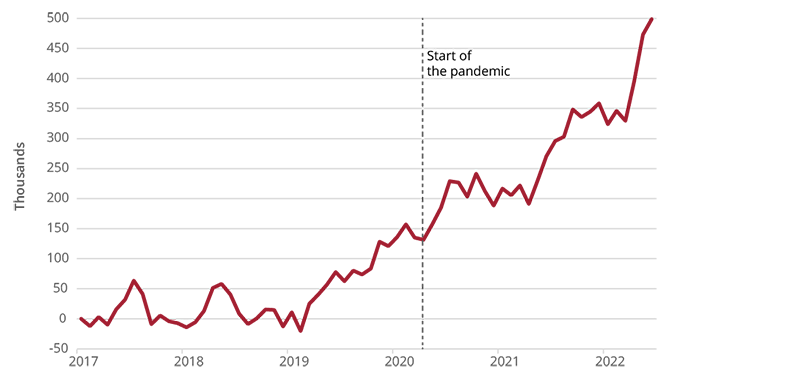
Figure 1. Cumulative change in the number of people aged 16-64 who are inactive due to long-term sickness. Source: Office for National Statistics.
COVID-19: Catalyst or Symptom?
While the pandemic undeniably worsened the situation, we shouldn’t ignore pre-existing trends. The ONS highlights that the rise in long-term sickness began before COVID-19 emerged. This suggests that the pandemic acted as a catalyst, exposing and exacerbating underlying health issues within the population.
Long COVID itself has played a significant role. Studies, including one published recently in JAMA Psychiatry, indicate that a substantial proportion of individuals who contract COVID-19 experience lingering symptoms that impact their ability to work. Conditions like ME/CFS (Myalgic Encephalomyelitis/Chronic Fatigue Syndrome), with an estimated prevalence of 250,000 in the UK, have seen a surge in diagnoses post-pandemic. This "shadow pandemic" of long COVID that contains within it, increasing evidence of vaccine-induced harms that were known to regulatory agencies (see the book just launched by Naomi Wolf, The Pfizer Papers, War Room Books, 632 pp.), that has added another very significant layer of complexity to the crisis.
Beyond the Virus: Exploring Contributing Factors
The reasons behind this surge are multifaceted. UK non-profit, the Health Foundation, emphasises the need to look beyond the immediate impact of the virus. They point to an ageing population, increasing prevalence of chronic conditions like mental health problems and musculoskeletal disorders, and persistent health inequalities as significant contributors. An increasing number experience two or more of these conditions at the same time (Fig. 2).
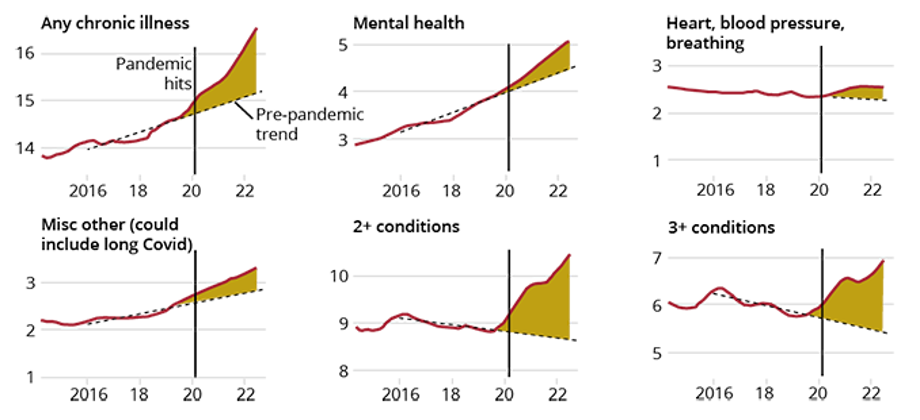
Figure 2. Share of all people aged 16-64 with selected long-term conditions (%). Source: Financial Times.
Furthermore, research from YouGov reveals a concerning trend of widespread fatigue in the UK, with one in eight Britons reporting feeling ‘tired all the time’, abbreviated in the medical profession to TATT. Another quarter report feeling weary ‘most of the time’, while a further third feel exhausted ‘about half of the time’. This pervasive fatigue could be indicative of underlying health problems, lifestyle factors that contribute to long-term sickness, as well as changes to the environments in which we live and are exposed.
International Comparisons
Data on long-term sickness in the UK are on average far from the worst among other countries (Fig. 3)
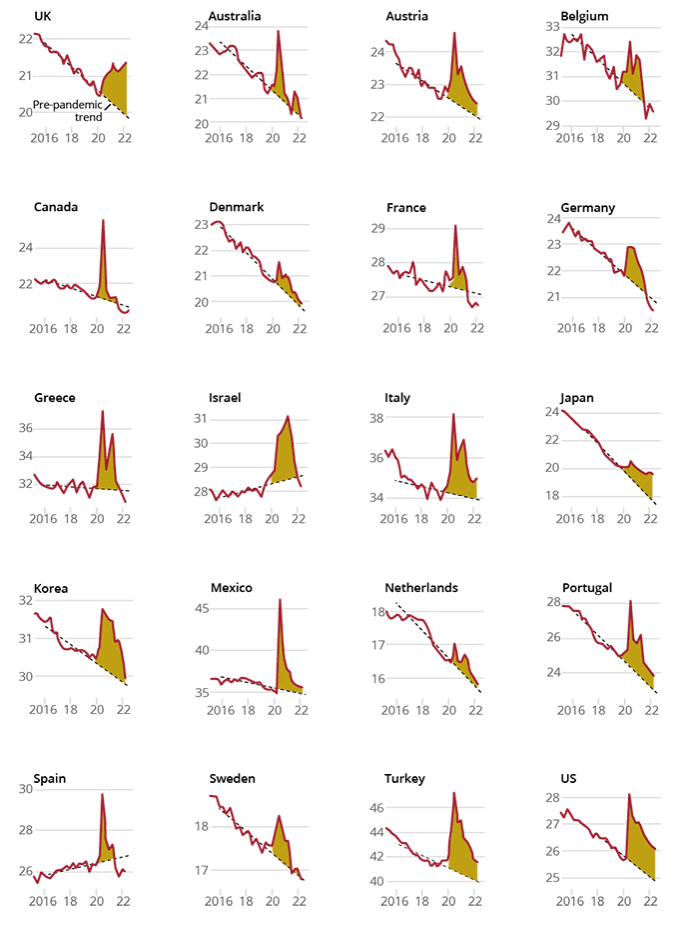
Figure 3: Comparison of economic inactivity rates among developed economies. Source: Financial Times.
The UK’s problem centres around the very thing that makes the “free” NHS, in the minds of many, the jewel in Britain’s welfare crown. This free access to care, regardless of your financial or health status, has made huge numbers dependent on it. The consequences of this, with so many people having unmet health needs, will disproportionately affect the most disadvantaged. This is well demonstrated in Fig. 4.
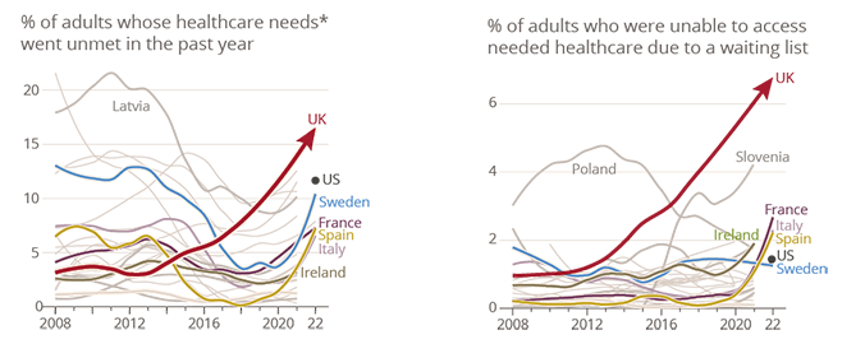
Figure 4: International comparison of survey responses for unmet care needs and waiting lists. Source: Financial Times.
Addressing the Crisis: A Call for Action
Tackling this multifaceted challenge requires a comprehensive and collaborative approach. As history has shown many times over, leaving this kind of a challenge to government will prove unsuccessful. This is more the case than ever before because of the intractable connection between governments, Big Pharma and global agencies such as the World Health Organization (WHO).
So many of the solutions that are needed are linked to decisions we make as individuals, not ones made in the corridors of government or the WHO. At the heart of a solution for so many is the need to re-connect with the diets and lifestyles that are closer to those of origin—yes, it’s all about natural health. However, there has never been a time in history where communication about these issues has been so gravely threatened: labelled by governments, the mainstream media and dominant social media platforms as misinformation or disinformation.
We’ve been working on a new model for bottom-up health care, our Regen Health Blueprint project that utilises a common language and operates within communities, for some years now. We’re working towards setting up validation trials for it—but right now, the focus has to be to defend free speech in healthcare so we can talk openly about the science and clinical benefits of natural health.
Sign our Freespeech4health petition NOW! (if you haven’t already)
There is copious evidence that disadvantaged communities often experience higher rates of chronic illness and face greater barriers to accessing healthcare. In the UK, this crisis that disproportionately affects those who need healthcare the most is at risk of breaking the economic, social and even spiritual ‘fabric’ of society. Yes, targeted interventions and support can help, but they are little more than band-aids.
Resolving this crisis has to be a priority for all of us if future generations are going to make it through. That means we have to be solution-focused at the level of the individual and community, among both conventional and alternative healthcare professionals and the systems within which they operate, at policy levels, and in the wide range of research fields that are touched by this crisis.
Protecting free speech, identifying the causes of the continuing spiral of long-term sickness and decline in the working population, as well as developing proactive, healthy and resilient individuals and communities is probably not a bad place to start. That’s our rationale for these being among our key focuses.
>>> If you’re not already signed up for the ANH International weekly newsletter, sign up for free now using the SUBSCRIBE button at the top of our website – or better still – become a Pathfinder member and join the ANH-Intl tribe to enjoy benefits unique to our members.
>> Feel free to republish - just follow our Alliance for Natural Health International Re-publishing Guidelines
>>> Return to ANH International homepage









Comments
your voice counts
There are currently no comments on this post.
Your voice counts
We welcome your comments and are very interested in your point of view, but we ask that you keep them relevant to the article, that they be civil and without commercial links. All comments are moderated prior to being published. We reserve the right to edit or not publish comments that we consider abusive or offensive.
There is extra content here from a third party provider. You will be unable to see this content unless you agree to allow Content Cookies. Cookie Preferences