One of ANH-Intl’s overriding missions is to help see a fundamental shift in how we manage health so that society’s overall approach is properly sustainable. That’s why we refer to sustainable healthcare. We talk a lot about it and over the coming weeks and months, as we prepare to release our landmark position paper, you’re going to hear even more about it. It’s big picture stuff that focuses the waking hours of people like us, but for many we know, as a concept, it’s just not close enough to home to be meaningful or feel relevant.
This article is intended to look at some simple approaches that could be readily introduced at the coalface of our healthcare system – in primary care, at the GP’s clinic. These could really help transform health outcomes by better predicting the potential onset of disease, or even more importantly, by providing sufficient foresight to allow disease to be prevented in the first place.
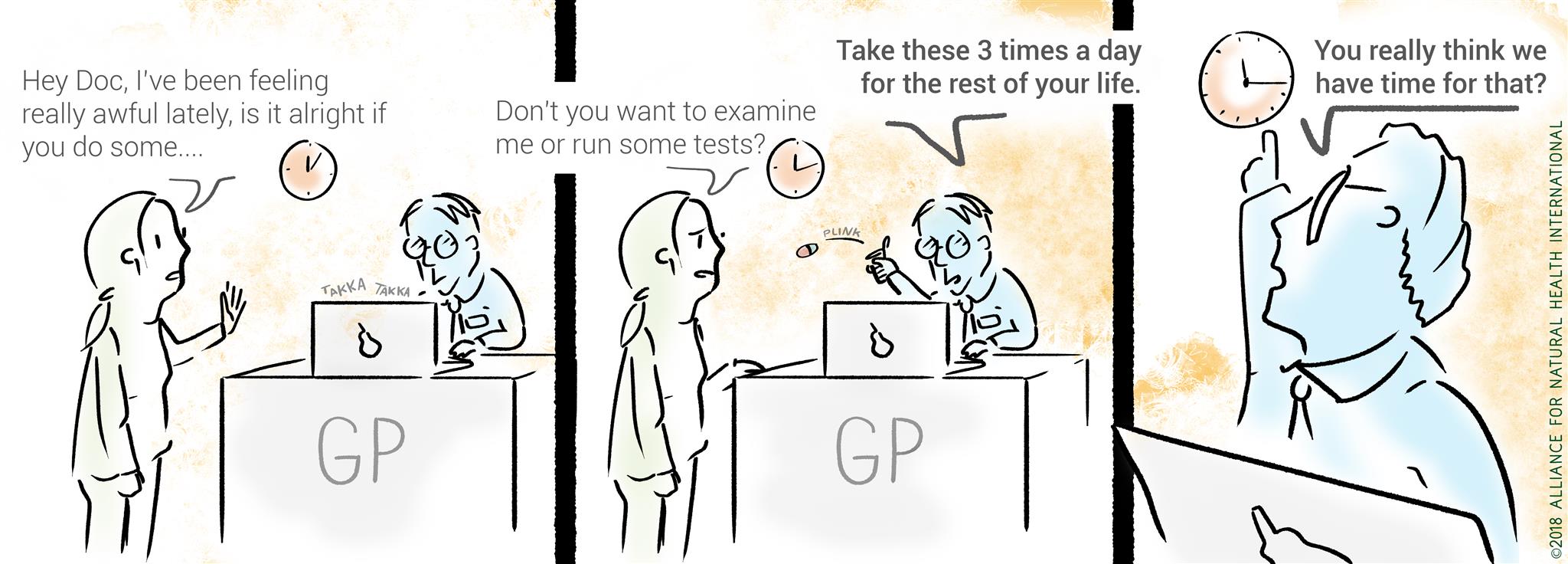
When you’ve had a taste of what Dr Leroy Hood describes as ‘P4 Medicine’ from an integrative or functional medicine practitioner it’s difficult to turn back. Having a bunch of new-to-nature chemicals thrown at you in the space of an 8-minute consultation replete with side effects no longer makes much sense. These integrative and functional approaches both use a systems biology approach to deliver healthcare that is Predictive, Preventative, Personalised and Participatory (hence P4) – the last P being the crucial key to unlock the door to success. Without us, as individuals first and patients second, being fully engaged in our own healthcare journey all falls to nought!
P for Predictive
Cardiovascular disease (CVD) and metabolic disorders (MD), such as obesity and type 2 diabetes, are tipping the chronic disease scales in the wrong direction. As such, we’ve singled out a selection of predictive methods that are common features of a more integrative (sustainable) approach to working with people who have or are at risk of developing CVD or MD. Yet these approaches have either fallen into disuse in mainstream primary care or they’ve never been introduced given that most primary care physicians spend most of their very limited time with patients prescribing drugs.
In this piece, we look at just 3 of the methods or approaches that we believe should be taken by all medical doctors in the frontlines of healthcare.
METHOD 1: Detailed and thorough case/medical history taking – those in a certain age bracket will remember when the doctor used to get up out of his/her chair and actually touch you whilst you were welcomed into the room. They looked at you, properly, taking you in and listening to what you were saying. There were no computer screens with drug databases to distract attention. A series of questions followed, detailed case history taking, the proper old-fashioned way whilst they continued to look at you, eliciting a world of information from your somatic cues (body language), body size, way your skin, hair and nails looked, how you walked and held yourself, the type of words you used to describe your problem, the light in your eyes, the vitality in your body and more. Then came the physical examination. The stethoscope round the neck, not just for show, but always feeling oh-so cold.
All this still takes place in the consulting rooms of an integrative/functional medicine practice. But it takes time and time is something conventional GPs don’t have. It’s why they’re glued to a computer screen most of the time matching symptoms to drugs. It’s not their fault, it’s all they have time for in an 8-10 minute consultation. But it’s not effective, it creates a rash of side effects, it’s a lost opportunity to help patient’s address the cause of their disease and condition, and, especially in the face of sky-rocketing chronic disease rates, fatigue-related issues, dementia and Alzheimer’s, it’s definitely not sustainable.
METHOD 2: Anthropometric testing – That’s a fancy way of referring to the measurement of bits of the body, be it height, waist, body composition or other parameters. By adding some inexpensive measurements to the information already gleaned from the initial examination session, an experienced practitioner has a world of information on which to base a clinical decision. What’s more, it’s personalised data.
Forget body mass index or BMI, the relationship between weight and height. The ratio between height and waist circumference (WHtR) gives a much better indication of a person’s risk of metabolic disease. If your waist measurement is more than half your height, you’re wading into high risk territory of metabolic dysfunction that can leave you vulnerable to a range of chronic diseases e.g. type 2 diabetes and CVD. It’s good to keep note of the chest and hip measurements too so that upward (or downward) trends in body size can be monitored over time.
Although everything to do with body weight appears to have been put in the non-PC ‘fattist’ basket, it cannot be ignored, despite GPs doing this routinely. From a health perspective it is not possible to carry additional adipose tissue (fat!) and not have some kind of metabolic disturbance e.g. increased inflammation, insulin resistance, mitochondrial (energy factories in cells) dysfunction, hormonal imbalance, dysbiosis, emotional mood swings, muscle and joint problems etc. To hear of cases where people are given the thumbs up and all-clear by their doctor in an annual health screen when they are clearly (and actually) grossly overweight is anathema to a functional medicine practitioner, but it happens all the time. That said, on the other end of the spectrum, dramatic and unexplained losses in body mass also need to be monitored.
With the advent of the new breed of bioelectrical impedance analysis (BIA) devices it’s now possible to glean detailed information on body composition e.g. percentage body fat, muscle mass, bone mass, cellular hydration, amount of visceral (angry) fat in the abdominal cavity round the organs and more. Most professional and advanced machines intended for home use will also give segmental readings for each arm and leg as well as the trunk to help monitor balance.
Alongside height and body measurements, BIA is an important instrument for health professionals. Its use can provide important data about body composition, in addition to complementary data about the clinical course of patients followed up on a medium- and long-term basis. It’s cheap and for many, replicable in their own homes, which makes it both sustainable and participatory.
METHOD 3: Functional testing through blood, urine, stool and saliva to elicit detailed information not only about current health status, but also to predict health trends with multiple tests over time. Here are just three examples:
- Organic Acids Test – this comprehensive metabolic screening involves the assessment of around 70 unique metabolites (markers) measured in urine. These markers are small, discarded organic acid molecules; by-products of human cellular activity, digestion of foods and the metabolism of gut bacteria. Some markers are produced by an overgrowth of gastrointestinal yeast and/or bacterial species due to impaired immune function or antibiotic use. Whilst laboratories do vary, a good Organic Acids profile should include evaluation of yeast and bacterial overgrowth, vitamin and antioxidant levels, fatty acid metabolism, neurotransmitter levels, metabolic ‘errors’, mitochondrial function, oxidative stress, detoxification and other key markers. Even with this brief overview, you can see how an experienced healthcare professional can add this level of detail to an increasingly wide, personalised, clinical view.
- Advanced lipid (fats) testing – Conventional lipid tests all too often focus only on total cholesterol (TC), triglycerides (TG), low-density lipoprotein cholesterol (LDL) and high-density lipoprotein cholesterol (HDL). Much is made of the total cholesterol reading as it’s the main determination for statin prescription, yet it’s the least robust or accurate marker of how the body is handling fat or of cardiovascular disease (CVD) risk. At the lowest level, the level of triglycerides and LDL are more important. However, real risk is associated with the tiniest particle sizes of LDL known as ‘very low density lipoproteins’ (vLDL) and then, mainly when they are oxidised. Most patients going through a conventional medical model will never have an advanced lipid test run on their blood to determine the different fractions of fats in their blood, their particle size distribution and least of all, the level of oxidation of the smallest particles. Parameters such as small dense low density lipoprotein (vLDL), oxidised low density lipoprotein (ox LDL), apolipoprotein A (Apo A1) and apolipoprotein B (Apo B) are rarely if ever measured conventionally, yet are standard procedure in functional medicine clinics with patients demonstrating red flags in their fat handling. Lifestyle changes such as weight loss, exercise, and dietary changes correlate with improvement in the profile of advanced lipoproteins. If these tests were more widely available so many at risk could be diagnosed faster and more accurately, be spared the risk of adverse side effects to unnecessary medication such as statins and be put on personalised lifestyle medicine protocols. The latter are not only much more effective than drug-based approaches, they are also much cheaper than drugs, giving another tick in the healthcare sustainability check box.
- Comprehensive thyroid function - Feeling ‘tired all the time’ (TATT) is a leading cause of why people visit their doctors. Given that the thyroid is the master controller of the hormonal system and also regulates metabolism, it's not surprising that thyroid testing has increased. Visit your conventional doctor displaying a major symptom of thyroid under activity (hypothyroidism), or over activity (hyperthyroidism), and you'll likely have just two markers run to determine thyroid function - T4 (thyroxine) and TSH (thyroid stimulating hormone). TSH is a pituitary hormone that monitors levels of thyroid hormone in the body. When the need increases, TSH tells the thyroid gland to release active hormone (T3, triiodothyronine) by converting T4. From the broader clinical perspective in functional medicine, these two hormones are insufficient markers to determine true thyroid function. In a comprehensive thyroid screen, by contrast, you'd find TSH, free T3, free T4 (free refers to the amount of hormone being used by the tissues), total T4 (the amount in 'storage'), reverse T3 (inactive), T3 uptake and thyroid antibodies, to check for the presence of autoimmune activity. In our increasingly hectic and stress-filled modern world, reverse T3 is coming into play more and more. It's the body's evolutionary 'safeguard', the brake on the system, when energy needs to be saved and channelled into more important systems like the immune system, on which survival depends. Reverse T3 has the ability to decrease active T3, bind to receptors and prevent what's left of the T3 getting in. It increases symptoms of hypothyroidism, yet doesn't change the T4 or TSH levels, which to your doctor, makes your thyroid function look normal and increases the likelihood of your symptoms being put down to a psychosomatic cause! With autoimmune diseases rising at a rapid rate, full functional thyroid screening is becoming more and more relevant given it's often the first predictive chink in the armour to show. Catch these things early and the chance for recovery is greatly enhanced before someone descends into full pathology. Again, another tick for preventative and sustainable.
Moving forward sustainably
Much of mainstream medicine today could be classified as preventative. But not in the positive sense of preventing disease. Rather, because its behemoth structure that’s deeply intertwined with Big Pharma prevents you from becoming an empowered participant in your own healthcare journey — and thus prevents you from becoming sustainably well.
P4 medicine and approaches like it that fully engage the individual is far from the magic bullet, pill for every ill, approach so beloved by Big Pharma. It’s all about understanding that our actions have consequences, but that our bodies are miraculous in their ability to rebalance and heal if we give each individual the resources and environment that he or she needs for repair. Using appropriate predictive methods such as case history taking (the old-fashioned way), anthropometrics, functional testing and observation is the first step to allow for preventative and personalised recovery programmes to be designed that engage and empower the patient so that they want to participate. It’s the people end of sustainable healthcare where the rubber meets the road!







Comments
your voice counts
28 February 2018 at 10:31 pm
What basic BIA device would you recommend for a clinician.
01 March 2018 at 12:19 pm
Hi Kate, my personal preference is Tanita as they have a good track record for reliability (+/-5% variance) and reproduciblility underpinned by valid science. They do a range of professional clinic versions and then some excellent ones for home use, that are also portable. You need to make sure that whichever device you use has handles to measure the full body. BIA devices that you just stand on only measure the lower half of the body and use algorithms to make an estimation on the rest. Omron is another company to look at, but I think they're more active in the consumer space. Feel free to email me ([email protected]) if you'd like any more info.
Best wishes
Meleni
01 March 2018 at 9:05 am
"Particle size? What's that?!? Never heard of it!" An NHS nurse recently revealed to me they had no idea about what particle size (type A large buoyant or type B small, dense) referred to. He (male nurse) humoured me when I showed him a copy of Dr Aseem Malhotra's article from the BMJ, 2013 titled 'Saturated fat is not the major issue' and pointed out where it describes LDL cholesterol particle sizes. He'd never heard of Dr Malhotra either. Dr Malhotra is an NHS cardiologist at Croydon Hospital, who flies the flag for healthier diets and lifestyles after seeing the light about how junk food doesn't help our health. [BMJ 2013;347:f6340 doi: 10.1136/bmj.f6340] This NHS nurse was simply doing his job within the conventional narrow-focus lipid tests. And he awarded me a clean bill of cardio health -- so, no threat of statins at least!
01 March 2018 at 1:15 pm
Thanks Isabella, it's a painful state of affairs isn't it? It's not the nurses or doctors' faults, they're doing their best in, as you say, the narrow confines of the conventional medical focus, but it's the patients who are losing out big time. That's where education comes in. The more people know, the more they can drive a system of healthcare that does actually support health and not just the drug industry. It's also where health professionals in the integrative/functional space come in as there's an army of us out there to support mainstream medicine if they would just crank open the door a bit further! As with any major shift in society, it will have to start from the grassroots with individuals demanding the type of healthcare they want rather than being told what's on offer.
Best wishes
Meleni
01 March 2018 at 10:16 am
A very valuable article. I think that one of the many issues surrounding how we as individuals take responsibility for our health, is that mentalities need to change drastically both within the health system as well as in how the patients relate to their own health.
01 March 2018 at 1:21 pm
Thanks for your comment Isabelle, great that you found it useful. As an integrative health practitioner of long-standing, I'm passionate about health empowerment and participatory healthcare. As you say, we need a major shift in focus so that individuals understand their role in their own journey back to health. At ANH, we feel that education is a key here, but there are still those who prefer the magic bullet solutions they believe are on offer. Unfortunately, there are no magic bullets when it comes to chronic diseases. The balance is tipping though and we believe there's a new healthcare dawn on the horizon. Watch out for our position paper on sustainable healthcare...
Best wishes
Meleni
12 March 2018 at 11:26 am
But actually finding a reasonably properly qualified integrative/functional medicine GP has proved hopeless. A body is needed with clear qualification guidelines so people can trust they are not being taken for a ride.
Your voice counts
We welcome your comments and are very interested in your point of view, but we ask that you keep them relevant to the article, that they be civil and without commercial links. All comments are moderated prior to being published. We reserve the right to edit or not publish comments that we consider abusive or offensive.
There is extra content here from a third party provider. You will be unable to see this content unless you agree to allow Content Cookies. Cookie Preferences