Content Sections
By Rob Verkerk PhD, founder, executive & scientific director
TOPLINE
- Health systems are breaking and governments and politicians seem to avoid looking at the underlying reasons for failure, and, instead, try to make us believe more funding, digital health and AI will come to the rescue
- While the reasons for failure are complex and multi-layered, most of them stem from two foundational problems: one is siloed thinking that’s part and parcel of medical reductionism that’s given us the prevailing biomedical model, and second is dirty money
- Mainstream health systems have been captured by pharmaceutical interests and don’t deliver or promote health, they are primarily sickness care systems that deliver products and services to sick people. Public health has been equally captured and then integrated into governmental health policies
- We’ve been developing a model for future fit, community health systems that are ecologically aligned, working with, not against, nature. We’re seeking conversations with people or organisations who might be able to help us with our next steps.
Listen to the article
Read the article
There’s no doubt this thing we call ‘healthcare’ is in crisis. Nowhere do we see this more clearly than in the world’s biggest healthcare system, the UK’s National Health Service (NHS). As many countries around the world move towards elections, fixing healthcare is high on the list of different parties’ political manifestos. Many politicians think the fix is going to happen simply by providing more funding — from taxpayers — while the techies out there are pinning their hopes on digital health and AI.
Taboo or not taboo
In a world in which taboos are created around almost any area that challenges the predominant flow of our so-called civilisation — one guided by the dominant corporate and political interests of the day — there are a bundle of root causes to healthcare failure that have become out-of-bounds in public parlance. You only have to try to launch a public debate that considers options to mass vaccination against COVID-19 to be aware of how these taboos work.
Taboos of this kind are manufactured by the corporate forces that control swathes of medical science and education as well as global communication networks. Conditioned by these unified perspectives, the main political parties, the educational institutions that train doctors and other health professionals, the administrators and bureaucrats that run ‘health systems’, the mainstream media that communicates to the public, and the social media that facilitate communication among the public, all end up carrying much the same kind of information. It all works on the premise that if you hear something often enough, you’ll start to think it’s the truth. Yes, our perception frames our sense of reality so if our perception is manipulated, so is our sense of the world around us.
What drives health?
But let’s drill down a bit. It’s been estimated that less than 20 percent of the health outcomes we experience in life are determined by the systems of clinical care with which we engage. The rest is down to the things we do in our daily lives, in our bedrooms, bathrooms, kitchens, and places of work. How long we sit, how we move, and for how long and how often. The nature of stress, how we respond to stress, how much we challenge ourselves to stretch our adaptive capacity. How much meaning we find in our lives, the degree of social and nature connection we feel and experience, and so much more.
Ironically, these are the very kinds of things the majority of clinicians whose task it is to improve health by preventing or treating disease tend to ignore. Some ignore these crucial determinants and influences on health unwittingly, through their lack of awareness of these issues, while others do it more deliberately, because it’s either too hard, they haven’t acquired the relevant skills, or it’s just too time consuming.
We then need to ask ourselves the question: how did we get to this place?
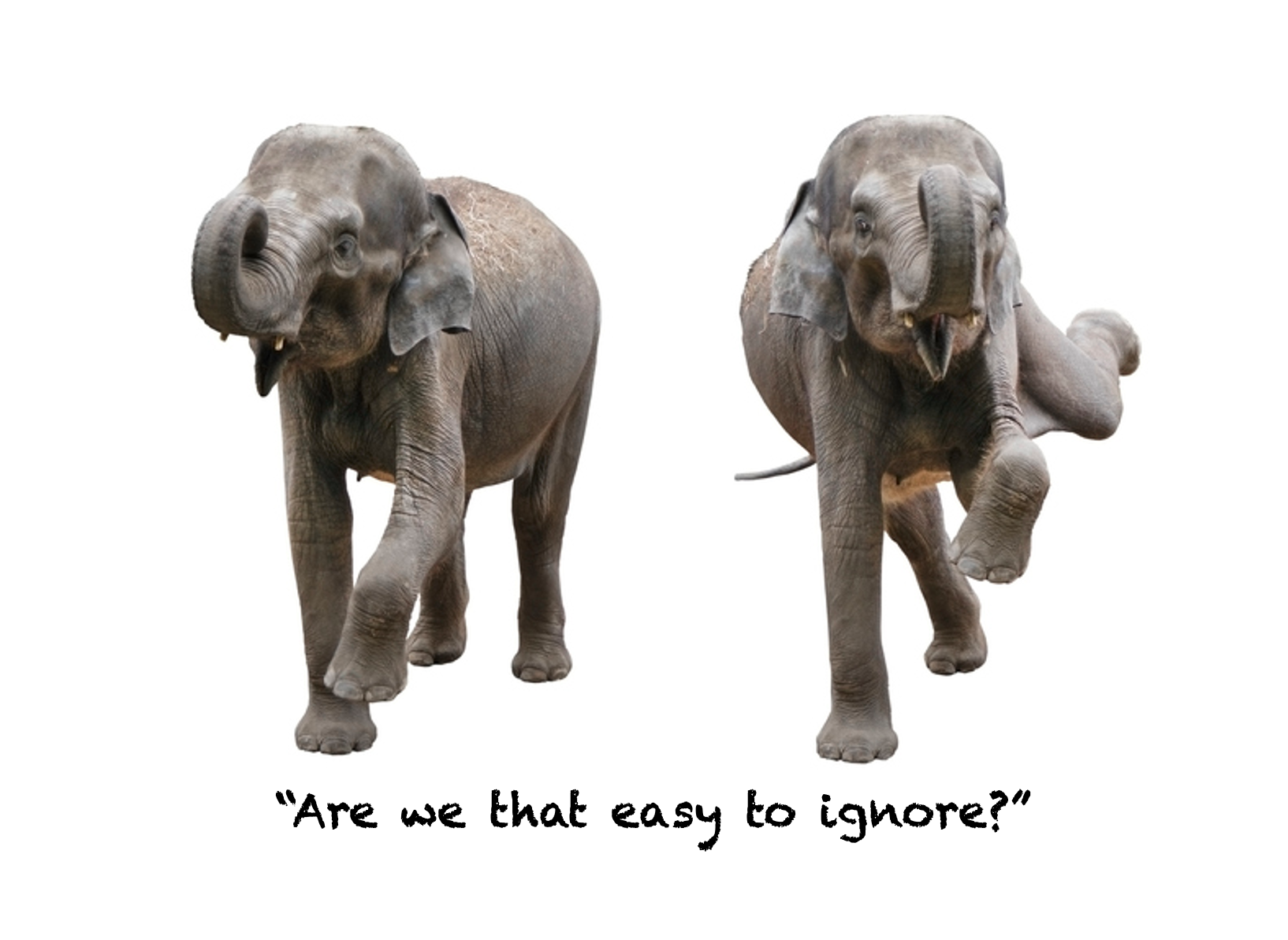
Two elephants in the room
I want to outline two very fundamental issues that underlie most other reasons. Those of us interested in co-creating health systems that work with, not against, nature, need to understand these reasons sufficiently well to ensure they’re excluded from the new systems that are so badly needed by society.
If we want future fit health systems for coming generations, we actually need to pull our communal fingers out and get on with it, such is the scale of the coming cascade of ill health and disease that is part and parcel of a maladapted, ageing population in an increasingly polarised and disconnected world.
Ironically, recent advances in our understanding of the human being and our species’ evolutionary background should make us more adept than ever before at dealing with these problems. But unfortunately, the increasingly controlling, authoritarian systems that govern the direction of societies across the globe have huge influence on how we tackle our myriad challenges. Economist Intelligence estimates that just 8 percent of the world’s population now live in full democracies, while 55% are ruled either by authoritarian or hybrid regimes. The rest, a substantial 37 percent, live in flawed democracies.
Failure Point 1: Disconnected siloes
Amongst the most important reasons for the structural turmoil being experienced by ‘healthcare systems’ is the siloed nature of the modern, Western scientific thinking as applied to medicine, one that has led to deep specialisation, typically at the cost of holism. It has delivered biomedical reductionism which is firmly woven into the DNA of the contemporary mainstream medical system. This desire and capacity of humans to delve deep into the siloes of knowledge and human endeavour has undoubtedly helped save countless lives, especially in the delivery of acute care. But it has also induced great harms, including death, with prescription medicines now estimated as the third leading cause of death after heart disease and cancer.
Just as relevant, the medical mainstream’s biomedical reductionism finds itself very poorly adapted to our current predicament of ageing populations in industrialised countries, which face an overwhelming and growing burden of chronic and mental health conditions. In part this is because hyper-specialisation has occurred in the absence of an adequate effort to address cross-, trans- and inter-disciplinary issues. This has limited the ability to see the big picture and, in particular, the incredible importance of connection between exquisitely interconnected and networked biological and energetic systems.
Here's the nub of it: it is the increasing and seemingly unappreciated disconnection of these systems, not the absence of the right cocktail of drugs or any missing technology, that is the central culprit in society’s escalating sickness.
Failure Point 2: Dirty money
The second big underlying reason for the increasing failure of the prevailing mainstream biomedical model is its intractable connection to corporate, most notably pharmaceutical and vaccine, interests. Yes, it might seem like a taboo to claim Big Pharma is dirty, but it is a corporate venture riddled with a history of fraud and illegal conduct, most recently exemplified by the $26 billion settlement agreed by 4 leading drug makers over their role in generating today’s opioid crisis.
It's not just the Big Pharma corporations that are the problem. It’s also all those organisations and individuals that are fuelled by Big Pharma’s money. That includes the people who run governments, agencies and political committees who have equity in these corporations. It’s the mainstream media outlets that depend on advertising revenues from Big Pharma as their lifeblood. And it’s also the cancer and other medical charities which have become fronts for pharma.
Together, these interests have distorted most people’s perception of what health care (and even health itself) is all about, making it synonymous with the delivery of clinical care and especially pharmaceutical medicines (recall my opening sentence which referenced research showing clinical care amounts to only 20% of health outcomes).
As a result, the system of ‘healthcare’ that most people rely on has little to do with caring for people’s health. It’s primarily to do with delivering products and services to sick people, so would better be described as sickness care.
Multiple books have been written about the capture of the medical-industrial complex by Big Pharma, among them that of former editor of the New England Journal of Medicine Marcia Angell, in her treatise, The Truth About the Drug Companies (Penguin Random House, 2005). Another, Cochrane co-founder Peter Gotszche’s Deadly Medicines and Organised Crime: How Big Pharma Has Corrupted Healthcare (CRC Press, 2013).
Since the organic chemistry revolution took off in the mid-20th century and it was learned that uniquely modified molecules could be patented, the pharmaceutical industry has had a deep preoccupation with the use of chemical solutions to treat human bodies and minds, these seen largely as biochemical machines. Medical doctors, researchers and even patients have come to assume the body needs these chemicals for healing to occur; compounds that are typically patented, new-to-nature chemicals to which there has been insufficient time for adaptation. This is actually a perverse concept when viewed from an evolutionary perspective. Surely it cannot be that denying our inherent requirement for a pharmaceutical drug is the main reason for so much sickness, and that sickness will be remedied if more people got more access to more drugs? (Look what happened with opiods…)
So let’s flip to what we do about the things that affect 80% of health outcomes, the things outside clinical care. In the spotlight here is part of the mainstream medical system that’s meant to do the heavy lifting in the field of health promotion. It’s far also from independent of corporate interests and it’s also inexorably linked to the medical-industrial complex, and even more tightly interwoven into government policy. It’s called ‘public health’, and it’s a multi-disciplinary approach that had its origins in a laudable concept first formulated in the 1920s, being the “science and art of preventing disease”. As big as this system has become, it is also well and truly captured.
You want evidence? The cholesterol myth that created ‘statin nations’, and the low fat myth that turned millions into sugar and opioid addicts are just two of many examples.
But it goes further still.
This is actually a very fundamental point and one that distinguishes two distinct, lop-sided foundational approaches to managing human health. One side, by far the weightiest and most influential, is the arena of the medical-industrial complex, which has also been considered a medical-education-industrial complex. It has encouraged a very limited perspective on the workings of the human body and mind. It has created the expectation that diseases need to be diagnosed via characteristic symptoms and then treated with a pharmaceutical, typically in pill form, or by surgery. It’s an approach that elevates the health practitioner, typically a medical doctor who has received a very specific kind of medical education, into an exclusive and esteemed position in society, as a technocrat who has the right to deliver technologies that are out of bounds, too difficult to understand and potentially risky in the wrong hands, that mere mortals who have not had sufficient training, or acquired a drug prescription license, should not be allowed free access. This group invariably believe to its core that technology fixes are where the real solutions to our health crisis lie.
Unsurprisingly, there’s another group to which you, dear reader, might belong. It is more diminutive in size, in status, and in influence, and it includes those who recognise the intrinsic power of self-regulation or self-healing (an intrinsic tendency of the body to achieve homeostasis under the right conditions) that exists in every organism. Those of us who are advocates of what we might call a ‘natural health first’ approach tend to be keen to work with the incredibly sophisticated homeostatic and epigenetic regulatory systems we’ve evolved over millennia. This allows us to fine tune the way our genes express themselves at a given time in our lives in a given environment, ones that that we can often change both internally and externally to facilitate this process. The reason so many people suffer what are often called preventable chronic conditions is that we are maladapted to the modern world. KPNI founder Leo Pruiboom’s Pruimboom Institute tackles this issue head on with its Intermittent Living concept.

Birthing a new health system
These two basal problems, that in turn generate a whole host of the problems we find in mainstream health systems have been completely factored out of the new health system model we have designed and are preparing to build and evaluate.
We published our ‘Blueprint for health system sustainability’ at the end of 2018, having started generating and evaluating ideas for it almost a decade earlier (see my JACNEM paper, 2009; “Can the Failing Western Medical Paradigm be Shifted Using the Principle of Sustainability?”.
We’ve been working behind the scenes on ways of translating these concepts into a real-world demonstration so that we can properly evaluate how a democratised, bottom-up, community health system, free of siloed thinking and unethical financial influence works in the real world. A system that relies on a common language for health that works across all modalities and that is also understood by empowered individuals. A system that is connected, not just digitally, but one that is built around our ecological health system, and is connected both socially and environmentally, including to natural systems.
We’ve designed a blockchain system that has the capacity to hold all our health data, whether from the allopathic medical system or our ecological health system. It is sovereign, and each individual will have the sole right to determine with whom these data are shared. We’ve found an incredible team who can build the system, but they can’t do it for free.
As I write this, we’re looking for funding or investment to build the blockchain system, so please contact [email protected] if you’re interested in talking to us about the opportunity.
We look forward to telling you more about these and related developments as 2024 progresses.
>>> If you’re not already signed up for the ANH International weekly newsletter, sign up for free now using the SUBSCRIBE button at the top of our website – or better still – become a Pathfinder member and join the ANH-Intl tribe to enjoy benefits unique to our members.
>> Feel free to republish - just follow our Alliance for Natural Health International Re-publishing Guidelines
>>> Return to ANH International homepage








Comments
your voice counts
There are currently no comments on this post.
Your voice counts
We welcome your comments and are very interested in your point of view, but we ask that you keep them relevant to the article, that they be civil and without commercial links. All comments are moderated prior to being published. We reserve the right to edit or not publish comments that we consider abusive or offensive.
There is extra content here from a third party provider. You will be unable to see this content unless you agree to allow Content Cookies. Cookie Preferences