As depression hits the news once again, and the number of worldwide depression sufferers continues to rise inexorably, new and effective approaches to treatment and management are clearly needed. Fortunately, a number of strategies already exist – no drugs required!
The ‘monoamine hypothesis’ of depression
Why do people suffer from clinical depression? Or more accurately, what is the underlying biological mechanism in people who suffer from clinical depression? The well-informed public, along with most healthcare professionals, would cite an imbalance of brain chemicals known as neurotransmitters. The recognised neurotransmitters involved in depression are serotonin, noradrenaline (norepinephrine) and dopamine, levels of which are manipulated by antidepressant medications.
These three neurotransmitters belong to a class of chemicals called monoamines, which lends itself to the popular name for the theory: the monoamine hypothesis of depression. And, while there are plenty of competing theories for the biological basis of depression, the monoamine hypothesis continues to reign supreme in the mainstream.
‘Disease mongering’ from day one?
It’s not difficult to understand why. The theory basically arose in reverse: rather than an experimentally testable hypothesis developing from systematic examination of a biological system, the monoamine hypothesis sprang from observations of improvements in depressed patients given monoamine drugs. In other words, pharma was there from the very start.
Professor Peter Götzsche, author of the must-read book Deadly Medicines and Organised Crime: How big pharma has corrupted healthcare cuts to the chase in an enlightening article that deconstructs 10 myths of psychiatry. Myth 1 is “Your disease is caused by a chemical imbalance in the brain”; Prof Götzsche continues, “Most patients are told this but it is completely wrong...the theories that patients with depression lack serotonin and that patients with schizophrenia have too much dopamine have long been refuted...There is no chemical imbalance to begin with, but when treating mental illness with drugs, we create a chemical imbalance, an artificial condition that the brain tries to counteract...Our citizens would be far better off if we removed all the psychotropic drugs from the market, as doctors are unable to handle them.”
For the full story, we heartily recommend reading the rest of Prof Götzsche’s article, the comments below it, the response from psychiatrist George Dawson and Prof Götzsche’s reply. And if you’ve got a few hours to spare, you could do worse than to explore the blog of psychiatrist, psychopharmacologist, scientist and author Prof David Healy, where the English version of Prof Götzsche’s article was published.
Better candidates needed
So if the ‘chemical imbalance’ theory is, at best, an enormous oversimplification, the question remains: what causes clinical depression? There are plenty of candidates out there that doubtless work in combination to produce clinical depression, but huge amounts of evidence are piling up to support crucial roles for the gut, gut bacteria and our relationship with microbes in the world around us.
The bane of the ‘grain brain’ brain drain
Increasing numbers of people, including mainstream physicians, are recognising that gluten is a health no-no responsible for an ever-lengthening roll call of problems – regardless of the presence of full-blown coeliac disease. As a dietary staple consumed several times a day in Western countries, wheat is a particular problem. In short, wheat and other gluten-containing grains trigger a cascade of biochemical inflammation that can manifest as such disparate conditions as urticaria and rhinitis, dermatitis herpetiformis, type I diabetes, rheumatoid arthritis, inflammatory bowel disease – and depression.
Research demonstrates an independent association between gluten and depression in patients with non-coeliac gluten sensitivity (NCGS). Furthermore, adhering to a gluten-free diet significantly reduces depressive symptoms in patients with full-blown coeliac disease, in whom depression is over-represented compared with the general population. Dr David Perlmutter’s book Grain Brain is a great source of information on this topic, and The Gluten Summit really takes things to the next level.
Leaky gut and inflammation
Perhaps the most important mechanism by which wheat and gluten give rise to inflammation is increased gut permeability. A so-called ‘leaky gut’ results in gut bacteria and other molecules that should be restricted to the digestive tract passing through the intestinal wall and into the bloodstream. Not surprisingly, these unwanted visitors set up all kinds of autoimmune biological reactions in the body, most of which have inflammation at their core. Logically enough, since depression is an inflammatory condition, anti-inflammatory compounds such as curcumin – from turmeric – are proving at least partially successful in early clinical trials.
Reason from Prof Raison
According to researchers such as Professor Charles Raison, however, the role of bacteria in clinical depression may be even more crucial. You may have heard of the ‘hygiene hypothesis’, which suggests that our present obsession with sterility and germ-free environments, and our over-use of antibiotics in particular, lies at the heart of numerous health problems. We’re just too clean, basically. Taking the hygiene hypothesis a step further, Prof Raison believes that our co-evolution with many species of environmental microbes trained our immune systems to tolerate constant, low-level immune challenges from these very organisms. He named his theory the ‘old friends’ hypothesis to acknowledge the benefits we receive from our invisible neighbours.
Atomic bomb vs. sniper
By taking our ‘old friends’ out of the equation through constant antibiotic use, says Prof Raison, we have broken a key line of communication between our immune system and the environment. The ‘atomic bomb’ of our innate immune system has taken over at the expense of the ‘stealth sniper’ of our adaptive immune system; an energy-intensive, messy recipe for systemic inflammation – and its consequences – over the long term. Prof Raison’s current research aims to treat patients with depression by reducing inflammation, using such strategies as whole-body hyperthermia.
Gardeners are happier – it’s official!
Intriguing research by Dorothy Matthews and Susan Jenks of The Sage Colleges in New York not only adds weight to the concept of communication between environmental bacteria and ourselves, but hints at a mechanism for why gardeners find their craft so uplifting. When the researchers gave mice food laced with the soil bacterium Mycobacterium vaccae, they found their way through a maze twice as quickly as normally fed controls. What’s more, they exhibited less anxiety-related behaviour, and the effects persisted for a week. The Sage research built on previous work from the UK, which found that heat-killed M. vaccae or its components increased serotonin production from certain brain areas. Since it’s unlikely that these effects are limited to M. vaccae, simply going into nature and breathing the microbe-rich air will produce an antidepressant effect. No wonder that the evidence indicates that outdoor exercisers reap more wellbeing benefits than gym bunnies!
Gut–brain information superhighway
Depression may also be caused by direct communication between our brain and our gut, often termed our ‘second brain’. Current research points to three coexisting and complementary mechanisms through which our gut talks to our brain (Figure 1): via neurotransmitters such as serotonin, via signalling molecules known as cytokines and via the vagus nerve. Now that science is catching up with natural healthcare by recognising that diet can alter the microbial population in the gut, a clear mechanism exists for how a disordered gut microbiota, AKA dysbiosis, could contribute to or even cause depression. And, since it’s a two-way communication channel between gut and brain (Figure 1), it’s easy to see how stress contributes to depression by driving alterations in gut flora and inflammation.
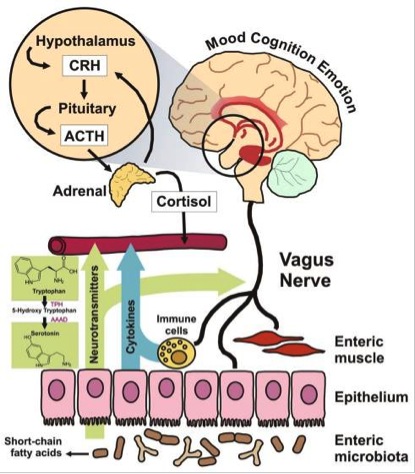
Figure 1. Mechanisms of bidirectional communication between the brain and the gut. Taken from Grenham S et al. Front Physiol 2011;2:94.
Community is key
As initiatives like the Human Microbiome Project (HMP) confirm the incredible number and variety of micro-organisms that share our bodies, it becomes clearer that each human being is an individual universe teeming with life. Indeed, what does it mean to be ‘human’ when commensal bacteria outnumber our cells by more than 10 to 1? As common sense should tell us, and as science is now confirming, human beings cannot operate to their fullest in the absence of direct interaction with the external universe – the infinite richness of nature itself. Just as importantly, the evidence is building that simple changes to diet and lifestyle have the potential to make enormous differences in people with clinical depression, without the need for drugs of any sort. So why not prioritise your nutrition, include regular outdoor active time and perhaps consider trying your hand at growing your own depression-busting, edible mood garden?








Comments
your voice counts
21 August 2014 at 4:59 pm
Fascinating article. There is Bi-Polar passing genetically through my family from my Mother's side. Bless her she has just passed away aged 93. Mum suffered with depression much of her life but was never diagnosed as Bi-Polar. Whereas my sister was diagnosed Bi-Polar and experienced disturbing halucinations. My sister having had several breakdowns, compounded by marriage problems, all three of her daughters have suffered emotional problems of varying severity with depressive symptoms I recognise from my three years of psycho-therapy in the mid nineties.
Interestingly, I suffer with leaky gut and have in recent years found Fenugreek Seed very effective in stemming the problem. My tinnitus is much reduced and my digestion more stable although still sensitive. I opt for gluten free food where possible. I originally thought this problem came from my father's side. Dad had delicate digestion, but maybe it is linked in to my Mother's family tree as well.
I use the adaptogen Ashwagandha and various other natural plant supplements to maintain my health sucessfully, whereas my sister uses or has used lithium.
I agree that our disconnection with nature and over protection from germs is reducing the human body's ability to resist disease. However I have reservations that "medicinal drugs" play a major role in triggering depression. I have never taken very many "medicinal drugs" in my lifetime and in practically none in the last 20 years. If I have dental infection, flu symptoms or stomach upset I reach for my Bee Propolis capsules. On correct dosage they work fast & effectively every time. Propolis does not kill good gut bacteria only the bad.
I think I must have saved the NHS thousands of pounds over the years. If only the NHS were not in the pockets of Big Pharma, tax payers could save millions and avoid attracting super bugs with Big Pharma's anti-biotics.
Anyway I rest my case for now.
11 October 2014 at 10:18 am
Fascinating. Esp the effect of soil and even air micro organisms. Strong evidence that we were made from everything else and that if we aren't part of it any more, we can't be well
24 June 2017 at 10:30 am
So much of this information applies to me. Stomach disturbances post spinal surgery anaesthesia sent me spiralling towards anti depressants. Since then its been a roller coaster, psych wanting to augment anti deps with anti psychotics, no signs of bipolar though. Absolutely frightened to death over all this i find no help anywhere else. What on earth can a person do to get back to normal life. Dr david healy seems to have hit nail on the head. Lets try to get some of his work put into practice.
05 September 2017 at 1:18 pm
After 10 days of chronic diarrhea I went into depression. Now on antidepressants for 2 years and still depressed with diarrhea every morning - 3 times. I feel my depression came about with my stomach problems but don know what to do next.
06 September 2017 at 9:03 am
Hello Shiraz, We're sorry to hear you're feeling very well.
A functional medicine practitioner will be able to help you look at dietary and lifestyle issues that may be contributing to your stomach problems. Here is a link to their find a practitioner page https://www.ifm.org/find-a-practitioner/.
I hope this helps.
Warm Regards
Melissa
Your voice counts
We welcome your comments and are very interested in your point of view, but we ask that you keep them relevant to the article, that they be civil and without commercial links. All comments are moderated prior to being published. We reserve the right to edit or not publish comments that we consider abusive or offensive.
There is extra content here from a third party provider. You will be unable to see this content unless you agree to allow Content Cookies. Cookie Preferences